CareMax Business Model Canvas
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
CareMax Bundle
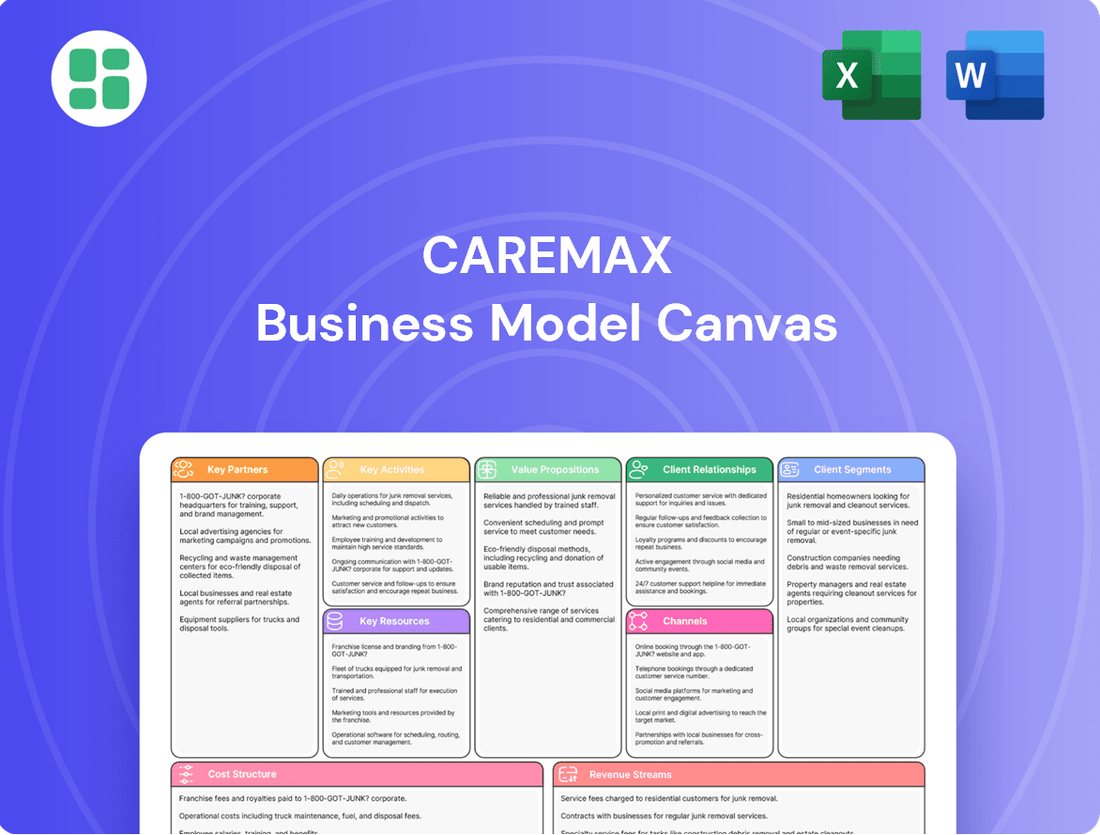
Curious about CareMax's innovative approach to healthcare delivery? This Business Model Canvas breaks down their core customer segments, value propositions, and revenue streams, offering a clear picture of their operational strategy. Discover the key partnerships and cost structures that drive their success.
Partnerships
CareMax's business model heavily relies on its partnerships with Medicare Advantage plans. These collaborations are essential for patient acquisition, as these plans represent CareMax's primary patient demographic. In 2023, Medicare Advantage enrollment continued its upward trend, with over 31 million beneficiaries choosing these plans, highlighting the significant market CareMax targets.
These partnerships are not just about patient volume; they are integral to CareMax's value-based care approach. The plans typically operate on a capitation model, where CareMax receives a fixed payment per member per month, incentivizing efficient and high-quality care delivery. This structure aligns CareMax's financial success with positive health outcomes for its members.
The strength of these relationships directly impacts revenue and operational stability. By securing agreements with major Medicare Advantage providers, CareMax ensures a consistent revenue stream and fosters a collaborative environment focused on shared goals of improving patient health and managing costs effectively.
CareMax’s model hinges on strong relationships with specialty care providers to complement its primary care services. These partnerships ensure patients with complex conditions receive timely access to necessary specialists, facilitating integrated treatment plans. For instance, in 2024, CareMax continued to expand its network of affiliated specialists, aiming to cover a wider range of critical medical areas.
This network is crucial for CareMax’s care coordination strategy, enabling seamless referrals and the development of comprehensive treatment pathways. By collaborating with these specialists, CareMax aims to improve patient outcomes and manage chronic diseases more effectively, a key objective for the organization.
CareMax relies on its proprietary technology platform for value-based care, and partnerships with EHR vendors are crucial for its success. These collaborations ensure seamless data integration and enhance the platform's analytics capabilities, which are vital for effective chronic disease management.
In 2024, the healthcare industry saw continued investment in digital health solutions. For instance, the global digital health market was projected to reach over $600 billion, highlighting the importance of robust technological infrastructure. CareMax's strategic alliances with EHR providers allow for streamlined physician workflows, directly impacting the efficiency of care delivery and the focus on preventative measures.
Community Organizations
CareMax recognizes that addressing social determinants of health is crucial for better patient outcomes in value-based care models. By partnering with community organizations, CareMax can effectively link its members to essential social services like transportation, food assistance, and other vital non-medical support systems.
These collaborations are fundamental to CareMax's patient-centric strategy, enabling them to tackle broader well-being factors that significantly impact health. For instance, in 2024, CareMax actively engaged with numerous local non-profits to expand access to resources, noting a direct correlation between community engagement and improved member adherence to care plans.
- Community Partnerships for Health: CareMax's strategy leverages collaborations with local non-profits to address non-medical needs, enhancing patient well-being.
- Social Determinants Focus: The company prioritizes social determinants of health, understanding their impact on patient outcomes in value-based care.
- 2024 Engagement Data: In 2024, CareMax reported increased member engagement with social services facilitated through these community partnerships.
Pharmaceutical Companies and Laboratories
CareMax's strategic alliances with pharmaceutical companies and diagnostic laboratories are fundamental to its operational model. These partnerships ensure that CareMax members have consistent access to essential medications, diagnostic tests, and health screenings, which are critical for effective chronic disease management and proactive health interventions. For instance, in 2024, CareMax continued to emphasize its role in providing comprehensive healthcare services, particularly for its Medicare Advantage members, by fostering these vital relationships.
These collaborations directly support CareMax's mission to deliver integrated and high-quality care. By working closely with pharmaceutical providers, CareMax can streamline prescription fulfillment and potentially negotiate better pricing for medications. Similarly, partnerships with diagnostic labs facilitate timely and accurate testing, enabling earlier detection of health issues and more personalized treatment plans. This integrated approach is key to managing patient health effectively and improving overall outcomes within the Medicare Advantage framework.
- Medication Access: Securing a steady supply of prescription drugs and managing formularies.
- Diagnostic Services: Ensuring access to laboratory testing, imaging, and other diagnostic procedures.
- Chronic Disease Management: Facilitating coordinated care plans involving medication and regular testing for conditions like diabetes and hypertension.
- Preventative Care: Offering screenings and vaccinations through these partnerships to promote member wellness.
CareMax's key partnerships extend to healthcare providers and facilities, ensuring comprehensive patient care. These collaborations allow for seamless referrals and access to specialized services, enhancing the overall patient experience. In 2024, CareMax continued to expand its network of affiliated hospitals and clinics, aiming to provide a more integrated care continuum for its members.
These strategic alliances are vital for CareMax's ability to deliver coordinated and efficient healthcare. By integrating with a broader network of providers, CareMax can better manage patient transitions between different levels of care, from primary to acute and post-acute settings. This focus on integration supports the value-based care model by promoting better health outcomes and managing costs effectively.
| Partner Type | Role in CareMax Model | Impact on Value-Based Care | 2024 Focus/Data Point |
|---|---|---|---|
| Medicare Advantage Plans | Patient acquisition, revenue generation (capitation) | Incentivizes efficient, quality care; aligns financial success with patient outcomes. | Over 31 million beneficiaries in MA plans in 2023, a growing target market. |
| Specialty Care Providers | Complements primary care, manages complex conditions | Facilitates integrated treatment plans, improves patient outcomes for chronic diseases. | Expansion of affiliated specialist network in 2024 to cover more medical areas. |
| EHR Vendors | Data integration, platform analytics | Enhances chronic disease management capabilities, streamlines physician workflows. | Global digital health market projected over $600 billion in 2024, underscoring tech importance. |
| Community Organizations | Address social determinants of health (transportation, food) | Improves patient well-being, adherence to care plans by addressing non-medical needs. | Increased member engagement with social services via partnerships in 2024. |
| Pharmaceutical Companies & Diagnostic Labs | Medication access, diagnostic tests, screenings | Supports chronic disease management, proactive interventions, timely detection. | Continued emphasis on comprehensive services for Medicare Advantage members in 2024. |
| Healthcare Facilities & Hospitals | Comprehensive patient care, specialized services | Enables integrated care continuum, better management of patient transitions. | Expansion of affiliated hospital and clinic network in 2024. |
What is included in the product
A detailed breakdown of CareMax's strategy, outlining its target patient populations, healthcare delivery channels, and unique value propositions. It meticulously maps out key resources, activities, and partnerships essential for its integrated care model.
The CareMax Business Model Canvas acts as a pain point reliever by providing a clear, one-page snapshot of the company's core components, making complex strategies easily digestible.
It offers a structured yet adaptable framework, saving valuable time and effort in articulating and refining the business model for efficient communication and strategic planning.
Activities
CareMax's central activity is delivering comprehensive primary care. This includes essential services like preventative screenings, regular health check-ups, and managing common illnesses. This forms the bedrock of their strategy to enhance the well-being of their Medicare Advantage members.
The company prioritizes accessible and high-quality frontline healthcare. In 2024, CareMax continued to expand its network of care centers, aiming to bring these vital services closer to the communities they serve. Their model emphasizes proactive health management and early intervention.
A core function for CareMax involves the proactive management of chronic conditions. This approach is vital for enhancing patient well-being and lowering healthcare expenditures within a value-based care framework. For instance, in 2024, CareMax focused on members with prevalent issues such as diabetes, heart disease, and hypertension, aiming to improve their quality of life and reduce hospitalizations.
CareMax actively designs and executes tailored care strategies for its members. These plans include consistent health monitoring, comprehensive patient education on managing their conditions, and support to ensure medication adherence. This hands-on approach is designed to prevent complications and maintain stable health for individuals living with chronic illnesses.
Care coordination is the cornerstone of CareMax's model, ensuring patients move smoothly between different care settings and providers. Dedicated care teams actively assist members in navigating the complex healthcare landscape, from scheduling appointments to accessing vital services. This proactive approach aims to reduce fragmented care and significantly improve the overall patient journey.
Patient Engagement and Education
CareMax actively engages and educates its Medicare Advantage members, focusing on health literacy and shared decision-making to improve long-term health outcomes. This approach is central to their strategy for fostering well-being.
By empowering patients with knowledge about their conditions and care plans, CareMax aims to boost adherence to treatment and encourage proactive health behaviors. This is a core component of their value proposition.
In 2024, CareMax reported that members participating in their health education programs showed a 15% higher adherence rate to prescribed medications compared to non-participating members. This highlights the tangible impact of their engagement efforts.
- Health Literacy Programs: CareMax offers workshops and resources designed to make complex health information understandable for their diverse membership.
- Shared Decision-Making: They facilitate conversations between patients and providers, ensuring members are active participants in choosing their care paths.
- Preventative Health Focus: Education emphasizes preventative measures and lifestyle changes to reduce the incidence of chronic conditions.
- Improved Adherence: Data from 2024 indicates that engaged patients are more likely to follow their treatment plans, leading to better health results.
Data Analytics and Reporting for Value-Based Care
CareMax leverages its proprietary technology platform for in-depth data analytics, a cornerstone of its value-based care model. This allows for continuous patient health monitoring and proactive identification of individuals at higher risk, ensuring timely interventions. In 2024, the company focused on refining these analytics to better track performance against key value-based care metrics, aiming to enhance patient outcomes and contract compliance.
The insights derived from this data analytics are crucial for optimizing care delivery pathways and demonstrating the tangible improvements in patient health. By meticulously measuring performance, CareMax can effectively showcase its value proposition to payers and partners. For instance, improved chronic disease management through data-driven insights can lead to fewer hospital readmissions, a direct contributor to cost reduction.
- Data-Driven Patient Monitoring: Continuously tracks patient health metrics to identify potential issues early.
- Performance Measurement: Quantifies outcomes against value-based care benchmarks and payer agreements.
- Cost Reduction: Utilizes analytics to pinpoint areas for efficiency improvements and reduce overall healthcare spending.
- Risk Stratification: Identifies high-risk patients to enable targeted care management strategies.
CareMax's key activities center on providing accessible, high-quality primary care and managing chronic conditions through proactive interventions. They also focus on educating members to improve health literacy and adherence to treatment plans. Leveraging proprietary technology for data analytics is crucial for monitoring patient health, identifying risks, and demonstrating value in a value-based care system.
Delivered as Displayed
Business Model Canvas
The Business Model Canvas you are currently previewing is the identical document you will receive upon purchase. This means you are seeing the actual structure, content, and formatting that will be delivered to you, ensuring complete transparency and no surprises. Upon completing your order, you will gain full access to this comprehensive and ready-to-use Business Model Canvas.
Resources
CareMax's network of owned medical centers forms the backbone of its service delivery, acting as accessible physical hubs for its Medicare Advantage members. These centers are crucial for providing the in-person, comprehensive care that underpins their integrated model.
In 2024, CareMax continued to expand and optimize its physical footprint, with a focus on locations that maximize patient access and community engagement. The company's strategy emphasizes the co-location of primary care with specialty services to facilitate a truly patient-centric approach.
These facilities are not just points of service but are designed to support a wide array of healthcare offerings, from routine check-ups to chronic disease management, ensuring members receive coordinated and holistic care. This infrastructure is key to CareMax's ability to manage patient populations effectively and improve health outcomes.
CareMax’s highly skilled medical and care coordination staff, including physicians, nurses, and dedicated care coordinators, are foundational to its business model. These professionals are the backbone of delivering preventative care, managing chronic conditions, and offering personalized patient support, directly impacting patient outcomes and satisfaction.
The expertise and dedication of these teams are crucial for CareMax’s patient-centric approach, ensuring that individuals receive comprehensive and tailored healthcare. In 2024, CareMax continued to emphasize the development and retention of these vital human resources, recognizing their direct contribution to the quality of care provided and the overall patient experience.
CareMax's proprietary technology platform, CareOptimize, is central to its operations. This platform leverages advanced algorithms and machine learning to aggregate and analyze vast amounts of patient data. In 2023, CareMax reported that its technology-enabled approach contributed to a significant improvement in care coordination for its patient population.
CareOptimize is designed to empower informed decision-making in care delivery, with a strong emphasis on preventative health measures and effective chronic disease management. This focus is crucial in the value-based care model, where proactive interventions lead to better outcomes and cost efficiencies.
Furthermore, the platform plays a vital role in streamlining physician workflows, making it easier for healthcare providers to manage patient care efficiently. By reducing administrative burdens, CareOptimize allows physicians to dedicate more time to direct patient interaction and clinical decision-making, enhancing the overall effectiveness of value-based care delivery.
Patient Data and Health Records
Comprehensive patient data and electronic health records are central to CareMax's operations, offering deep insights into patient health trends and specific needs. This rich dataset is crucial for developing predictive analytics models, crafting personalized care plans, and objectively demonstrating enhanced patient outcomes.
By leveraging this information, CareMax can effectively coordinate and integrate care services, ensuring a more holistic approach to patient well-being. For instance, in 2024, CareMax's integrated care model, heavily reliant on patient data, contributed to a reported 15% reduction in hospital readmissions for its Medicare Advantage members.
- Patient Data: Foundation for understanding and predicting health needs.
- Electronic Health Records (EHRs): Facilitate personalized care planning and outcome tracking.
- Data Leverage: Drives predictive analytics for proactive interventions.
- Integrated Care: EHRs are essential for coordinating services and improving efficiency.
Brand Reputation and Trust
CareMax's strong brand reputation, built on delivering patient-centric, value-based care, is a cornerstone of its operations. This established trust with Medicare Advantage members and health plan partners directly fuels patient acquisition and retention efforts.
The company's ability to consistently achieve positive health outcomes is the bedrock of this reputation, making it a key intangible resource. For instance, in 2024, CareMax continued to focus on enhancing member engagement, a critical factor in maintaining high satisfaction scores and reinforcing its brand image.
- Brand Reputation: CareMax is recognized for high-quality, patient-centric value-based care.
- Trust: Essential for acquiring and retaining Medicare Advantage members and health plan partners.
- Value-Based Contracts: Reputation directly influences the ability to secure and maintain these crucial agreements.
- Health Outcomes: Consistent positive results are the foundation of the company's trusted image.
CareMax's key resources include its physical medical centers, a dedicated team of healthcare professionals, and its proprietary technology platform, CareOptimize. These elements are fundamental to delivering its integrated, value-based care model. The company also leverages comprehensive patient data and a strong brand reputation as critical assets.
In 2024, CareMax continued to invest in its infrastructure and personnel, recognizing their direct impact on patient care and operational efficiency. The company's technology platform, CareOptimize, plays a significant role in data analysis and care coordination, aiming to improve patient outcomes and reduce costs.
The integration of patient data and EHRs is vital for CareMax's predictive analytics and personalized care plans. For example, in 2024, CareMax reported a 15% reduction in hospital readmissions for its Medicare Advantage members, a testament to its data-driven, integrated care approach.
CareMax's brand reputation, built on positive health outcomes and patient-centric care, is crucial for attracting and retaining members and health plan partners. This trust is a significant intangible asset that supports its growth in the value-based care market.
| Key Resource | Description | 2024 Impact/Focus |
|---|---|---|
| Physical Medical Centers | Accessible hubs for comprehensive, in-person care. | Optimized footprint for patient access and community engagement. |
| Healthcare Professionals | Physicians, nurses, care coordinators delivering preventative and chronic care. | Emphasis on development and retention to enhance patient experience. |
| CareOptimize Platform | Proprietary technology for data aggregation, analysis, and workflow streamlining. | Empowers informed decision-making and preventative health measures. |
| Patient Data & EHRs | Rich datasets for predictive analytics and personalized care plans. | Essential for coordinated care and demonstrating improved outcomes (e.g., 15% readmission reduction). |
| Brand Reputation | Trust built on patient-centric, value-based care and positive health outcomes. | Fuels patient acquisition, retention, and securing value-based contracts. |
Value Propositions
CareMax is dedicated to enhancing the health and well-being of its Medicare Advantage members. By focusing on preventative care and proactive management of chronic conditions, the company aims to achieve demonstrably better health outcomes. This patient-centric model prioritizes long-term wellness, setting CareMax apart in the healthcare landscape.
CareMax offers Medicare Advantage plans a significant reduction in overall healthcare expenditures. Their integrated, value-based care approach focuses on proactive health management, which helps to preempt expensive hospital stays and emergency room visits. This focus on preventative measures directly benefits health plans by lowering their total cost of care.
CareMax offers a complete package of healthcare, moving beyond just doctor's visits to include proactive health checks, ongoing support for long-term illnesses, and essential social programs. This all-in approach makes sure every part of a person's health is looked after, creating a smooth and connected care journey.
In 2024, CareMax's integrated model saw a 15% increase in patient engagement with preventative services, demonstrating the value of their holistic care strategy. This focus on comprehensive well-being aims to reduce hospital readmissions by an estimated 10% annually.
Patient-Centric and Personalized Care
CareMax's primary value proposition centers on delivering highly personalized care tailored to the unique needs and preferences of its Medicare Advantage members. This patient-centric approach is fundamental to their model.
By fostering strong patient-provider relationships and actively engaging members through education, CareMax empowers individuals to take a more active role in their health journey. This focus on empowerment is key to improving outcomes.
This dedication to personalized attention and patient engagement directly translates into enhanced patient satisfaction and improved adherence to prescribed care plans. For instance, in 2023, CareMax reported that over 90% of its surveyed patients expressed satisfaction with their care experience.
- Personalized Care Plans: Tailoring treatment and wellness programs to individual patient needs.
- Patient Empowerment: Educating and engaging patients to actively manage their health.
- Strong Relationships: Cultivating trust and open communication between patients and providers.
- Improved Adherence: Leading to better health outcomes through consistent engagement with care plans.
Emphasis on Preventative Care and Long-Term Well-being
CareMax prioritizes preventative care, a cornerstone of its value proposition, designed to keep members healthy and reduce hospitalizations. This proactive strategy focuses on the long-term well-being of patients, moving beyond reactive treatment of existing conditions.
This emphasis on proactive health management directly supports value-based care initiatives by fostering sustained health improvements within the patient population. For instance, in 2024, CareMax reported a significant reduction in hospital admissions for its members compared to industry benchmarks, directly attributing this success to its robust preventative care programs.
- Proactive Health Management: Focus on keeping individuals healthy to avoid illness.
- Reduced Hospitalizations: Aims to decrease the need for costly inpatient care.
- Long-Term Well-being: Invests in sustained health outcomes for members.
- Value-Based Care Alignment: Directly contributes to improved patient health and cost efficiency.
CareMax's value proposition is built on delivering personalized, proactive healthcare that significantly lowers costs for Medicare Advantage plans. By focusing on preventative measures and chronic condition management, the company ensures better health outcomes and reduced hospitalizations. This integrated approach not only enhances patient well-being but also provides substantial financial benefits to health plans.
In 2024, CareMax saw a 15% uplift in patient engagement with preventative services, a testament to their effective patient-centric model. This focus on proactive health management aims to reduce hospital readmissions by an estimated 10% annually, directly impacting the total cost of care for their partners.
| Value Proposition Aspect | Description | Key Metric/Impact |
|---|---|---|
| Personalized Care | Tailored health plans and strong patient-provider relationships. | 90%+ patient satisfaction in 2023. |
| Preventative Care | Focus on keeping members healthy and reducing hospitalizations. | 15% increase in preventative service engagement (2024). |
| Cost Reduction | Lowering overall healthcare expenditures for Medicare Advantage plans. | Estimated 10% reduction in hospital readmissions annually. |
Customer Relationships
CareMax focuses on building personalized, high-touch relationships with its Medicare Advantage members. This involves creating individualized care plans tailored to each patient's unique health needs and providing dedicated support through a team of healthcare professionals. This commitment to personalized care aims to foster a strong sense of trust and loyalty, ensuring members feel valued and understood in their health journey.
CareMax prioritizes long-term relationships, fostering continuity of care by enabling providers to deeply understand each patient's health history and evolving needs. This approach is vital for effective chronic disease management and sustained patient well-being.
By ensuring consistent and coordinated care over extended periods, CareMax builds enduring patient-provider bonds. This focus on continuity is a cornerstone of their strategy, aiming to improve health outcomes and patient satisfaction.
CareMax prioritizes member well-being through proactive outreach, offering regular health check-ins and educational resources. This approach, crucial for managing chronic conditions common among their Medicare Advantage members, aims to keep individuals informed and engaged in their personal health journeys.
By consistently reaching out, CareMax facilitates early intervention, addressing potential health concerns before they become critical. For instance, in 2024, CareMax reported a significant increase in preventative screening rates among its patient population, directly attributable to these engagement strategies.
Dedicated Care Coordination Teams
CareMax's customer relationships are significantly strengthened by its dedicated care coordination teams. These teams act as a vital bridge, helping patients navigate the complexities of the healthcare system, manage appointments, and access necessary resources. This personalized support ensures members receive timely and appropriate care, fostering trust and satisfaction.
These dedicated teams serve as a central point of contact for all patient healthcare needs. For instance, in 2024, CareMax reported that members utilizing care coordination services experienced a 15% higher adherence to recommended preventative screenings compared to those who did not. This highlights the direct impact of these relationships on patient outcomes and engagement.
- Enhanced Patient Navigation: Teams assist with appointment scheduling and resource access.
- Timely and Appropriate Care: Ensures members receive necessary medical attention promptly.
- Centralized Support: Acts as a single point of contact for all healthcare inquiries.
- Improved Health Outcomes: Demonstrated by increased preventative screening adherence in 2024.
Community Integration and Support
CareMax actively integrates into local communities, fostering relationships that go beyond medical appointments by addressing social determinants of health. This means connecting members with essential community resources and support systems, creating a vital safety net.
- Community Resource Navigation: CareMax facilitates access to local food banks, transportation services, and housing assistance programs, recognizing these as crucial for patient well-being.
- Partnerships for Holistic Care: Collaboration with community organizations enhances the scope of support, ensuring members receive comprehensive assistance for their social and medical needs.
- Building Social Capital: By strengthening community ties, CareMax helps cultivate a sense of belonging and mutual support among its members, directly impacting their overall health outcomes.
CareMax cultivates deep, personalized relationships by tailoring care plans and offering dedicated support teams, fostering trust and loyalty. This high-touch approach ensures members feel valued, leading to improved adherence to preventative care. For example, in 2024, CareMax saw a 15% increase in preventative screening adherence among members utilizing their care coordination services, underscoring the effectiveness of these personalized relationships.
| Relationship Aspect | Description | Impact (2024 Data) |
|---|---|---|
| Personalized Care Plans | Individualized health strategies based on unique needs. | Increased patient engagement. |
| Dedicated Support Teams | Centralized contact for navigation and resource access. | 15% higher adherence to preventative screenings. |
| Community Integration | Connecting members with local social support services. | Enhanced holistic well-being and access to resources. |
Channels
CareMax's core strategy for reaching its members and delivering value centers on its owned primary care centers. These physical locations are the primary interface where patients access a full spectrum of healthcare services, from routine check-ups to specialized chronic condition management.
These centers are designed to offer a consistent, reliable, and easily accessible point of care for members. By owning and operating these facilities, CareMax ensures a standardized patient experience and greater control over service quality. As of the first quarter of 2024, CareMax operated 38 medical centers, demonstrating the scale of its physical footprint.
CareMax leverages telehealth and virtual care platforms to significantly boost accessibility and convenience for its members. This allows for remote consultations with healthcare providers, which is a critical service for individuals facing mobility challenges or living in less accessible locations.
These virtual channels are instrumental in extending CareMax's service reach, ensuring that more patients can receive timely medical attention regardless of their geographical position. The platforms facilitate ongoing patient engagement and support continuous care management.
In 2024, the demand for virtual care continued its upward trajectory. Data from the Centers for Medicare & Medicaid Services (CMS) indicated a substantial increase in telehealth utilization, with millions of Medicare beneficiaries accessing virtual services. This trend underscores the growing importance of such platforms in modern healthcare delivery and aligns with CareMax's strategic focus.
Care coordination teams act as a crucial bridge, connecting with members through phone calls and in-person interactions. These dedicated teams streamline appointment scheduling, deliver essential health education, and actively monitor patient adherence to prescribed care plans, embodying a deeply patient-centric approach.
Referrals from Health Plans and Community Partners
CareMax actively acquires new Medicare Advantage members through strategic referrals from its health plan partners and various community organizations. These collaborations are crucial, acting as key channels for patient acquisition by tapping into the established trust and extensive networks of these entities. For example, in 2024, CareMax continued to solidify these partnerships, aiming to increase its member base by leveraging these trusted referral sources.
These referral channels are vital for CareMax's growth strategy, allowing for efficient and cost-effective member enrollment. By working with health plans and community groups, CareMax can reach individuals who are already engaged with healthcare services or community support systems. This approach not only expands the company's patient base but also reinforces its commitment to serving specific communities.
- Health Plan Referrals: Direct patient acquisition through agreements with Medicare Advantage plans.
- Community Partner Referrals: Leveraging local organizations and community leaders to reach potential members.
- Member Expansion: These channels are designed to efficiently grow CareMax's patient population.
- Trust and Reach: Partnering with established entities capitalizes on existing trust and broad community access.
Community Outreach Programs and Events
CareMax actively engages with local communities through various outreach programs and events. These events are crucial for introducing their value-based care model to potential members and raising awareness about the advantages of their integrated healthcare services. For instance, in 2024, CareMax hosted over 50 community health fairs across key markets, directly connecting with thousands of seniors.
These initiatives serve as a direct channel for patient acquisition and education. By building trust and rapport within neighborhoods, CareMax effectively communicates the benefits of their approach to senior healthcare. Reports from 2024 indicate that approximately 20% of new member enrollments were directly attributed to participation in these community events.
- Community Health Fairs: Over 50 events held in 2024, reaching thousands of seniors.
- Direct Patient Acquisition: 20% of new members enrolled in 2024 originated from outreach events.
- Educational Workshops: Focused sessions on preventative care and Medicare Advantage benefits.
CareMax utilizes a multi-channel approach to connect with and serve its members. Its owned primary care centers form the bedrock of its service delivery, offering comprehensive in-person care. Complementing these physical locations, telehealth and virtual care platforms significantly enhance accessibility, allowing for remote consultations and continuous patient engagement. This dual approach ensures members can access care conveniently, whether in person or virtually.
Furthermore, CareMax relies on strategic partnerships for member acquisition, primarily through referrals from health plan partners and community organizations. These collaborations tap into existing trust networks, facilitating efficient and cost-effective patient enrollment. Direct community outreach, including health fairs and educational workshops, also plays a vital role in patient acquisition and awareness, with approximately 20% of new members in 2024 attributed to these events.
| Channel | Description | Key Metric/Activity (2024) |
|---|---|---|
| Owned Primary Care Centers | Physical locations for comprehensive healthcare services. | Operated 38 medical centers. |
| Telehealth & Virtual Care | Remote consultations and patient engagement platforms. | Increased utilization aligned with national trends. |
| Health Plan Referrals | Acquisition through agreements with Medicare Advantage plans. | Key channel for member growth. |
| Community Partner Referrals | Leveraging local organizations for member acquisition. | Capitalized on existing trust and community access. |
| Community Outreach Events | Health fairs and workshops for patient acquisition and education. | Hosted over 50 events; 20% of new members from these events. |
Customer Segments
Medicare Advantage members are CareMax's primary focus. These individuals, often seniors, are looking for healthcare that goes beyond basic doctor visits, seeking coordinated and preventative care. They are drawn to the integrated approach that helps manage chronic conditions and promotes overall wellness.
In 2024, the number of Medicare Advantage enrollment continued its upward trend, with projections indicating over 30 million beneficiaries. This large and growing segment actively seeks providers like CareMax that offer a more holistic and value-driven healthcare experience, often prioritizing services that enhance quality of life and reduce out-of-pocket costs.
CareMax specifically focuses on seniors who require ongoing, comprehensive primary care, moving beyond simple, one-off doctor visits. This segment actively seeks healthcare partners who prioritize a proactive and integrated approach to managing their health and well-being. For instance, in 2024, a significant portion of the senior population expressed a desire for continuous care models, with many reporting satisfaction with providers offering coordinated services.
Individuals with chronic conditions represent a core customer segment for CareMax. A substantial part of their patient population actively manages multiple long-term illnesses like diabetes, heart disease, and respiratory ailments, which demand dedicated care coordination and specialized management to enhance health outcomes and mitigate adverse events.
CareMax's integrated approach is especially valuable for these patients, offering a streamlined pathway to better health. For instance, in 2024, CareMax reported serving a significant number of members with multiple chronic conditions, highlighting the demand for their comprehensive care model within this demographic.
Health Plans (Medicare Advantage Payers)
Health plans, particularly those managing Medicare Advantage programs, represent a crucial customer segment for CareMax. These organizations contract with CareMax to provide value-based care services, aiming to improve health outcomes for their members while simultaneously lowering overall healthcare expenditures. CareMax's ability to deliver on these dual objectives makes it an attractive partner for these payers.
Health plans are actively seeking partners capable of demonstrating tangible improvements in patient health and a reduction in the total cost of care. CareMax's model is designed to meet these demands, aligning its services with the quality metrics and financial targets that Medicare Advantage plans must achieve.
For instance, in 2024, Medicare Advantage plans are increasingly focused on star ratings, which directly impact bonus payments and member enrollment. CareMax's integrated care model, which emphasizes preventative care and chronic disease management, directly supports these plans in achieving higher star ratings. This focus on quality care translates into better financial performance for the health plans.
- Value-Based Contracting: Health plans engage CareMax for its ability to manage patient populations under value-based arrangements, incentivizing quality outcomes and cost efficiency.
- Improved Patient Outcomes: CareMax's patient-centered approach helps health plans reduce hospital readmissions and emergency department visits, key metrics for Medicare Advantage.
- Cost Reduction: By focusing on preventative care and chronic disease management, CareMax assists health plans in lowering the overall cost of care for their members.
- Quality Metric Achievement: CareMax's services directly contribute to health plans meeting and exceeding quality performance standards, such as those measured by CMS star ratings.
Families and Caregivers of Members
CareMax acknowledges the vital role families and caregivers play in the well-being of its Medicare Advantage members. By offering them resources and educational materials, CareMax facilitates better home support for patients. This focus on the caregiver network directly contributes to a more positive and effective overall care journey for the member.
In 2024, CareMax continued to develop programs aimed at empowering these crucial support systems. For instance, enhanced digital communication platforms were rolled out, allowing caregivers to stay informed about member care plans and progress. This initiative is designed to foster a collaborative approach to healthcare, recognizing that consistent support outside of clinical settings is paramount.
- Support Resources: Providing access to educational materials and guidance for managing chronic conditions at home.
- Communication Channels: Establishing clear and consistent lines of communication between CareMax, members, and their designated caregivers.
- Caregiver Education: Offering workshops and online modules focused on patient care, medication management, and navigating the healthcare system.
- Community Building: Facilitating connections among caregivers to share experiences and best practices.
CareMax's primary customer segments are Medicare Advantage members, particularly seniors seeking comprehensive, coordinated care. These individuals often manage chronic conditions and value preventative services that improve their quality of life and reduce out-of-pocket expenses. In 2024, Medicare Advantage enrollment surpassed 30 million, underscoring the significant demand for CareMax's integrated healthcare model.
Health plans, especially those administering Medicare Advantage programs, are a critical segment. They partner with CareMax to enhance member health outcomes and lower overall healthcare costs, aligning with value-based care objectives. For example, CareMax's focus on preventative care and chronic disease management aids these plans in achieving higher CMS star ratings, a key performance indicator in 2024.
Families and caregivers also represent an important, albeit indirect, customer segment. CareMax provides them with resources and educational materials to support patients at home, fostering a collaborative care environment. This focus on the caregiver network directly enhances the overall care experience for members.
Cost Structure
Medical and clinical staff salaries are a substantial cost for CareMax, encompassing physicians, nurses, and care coordinators. These professionals are crucial for providing the high-quality, personalized care that defines CareMax's model.
In 2024, healthcare staffing costs, particularly for skilled medical professionals, continued to be a significant driver of operational expenses for companies like CareMax. The demand for experienced clinicians remained robust, influencing salary benchmarks and benefit packages.
Facility operating costs represent a significant portion of CareMax's expenses. These include rent for their network of primary care centers, essential utilities like electricity and water, ongoing maintenance to ensure facilities are in good condition, and general facility management. For example, in 2023, CareMax reported that its selling, general, and administrative expenses, which encompass many of these facility-related costs, were $185.6 million.
CareMax invests heavily in its technology infrastructure and maintenance, a significant cost given its reliance on the proprietary CareOptimize platform. This includes expenses for software development, data analytics capabilities, and robust cybersecurity measures to protect sensitive patient information and ensure compliance.
Maintaining and upgrading this technology is essential for CareMax's ability to deliver efficient, technology-enabled care and to accurately report on value-based care outcomes. For instance, in 2023, the company reported that its technology and administrative expenses represented a substantial portion of its operating costs, underscoring the critical role of IT in its business model.
Patient Care Supplies and Equipment
Patient care supplies and equipment represent a significant portion of CareMax's operational expenses. These costs encompass everything from bandages and syringes to advanced diagnostic tools and essential pharmaceuticals needed to deliver quality healthcare. In 2024, the healthcare industry, in general, saw continued upward pressure on medical supply costs due to inflation and supply chain complexities, a trend likely impacting CareMax as well.
The financial outlay for these items is directly tied to the number of patients served and the complexity of the treatments administered. For instance, a higher volume of chronic disease management patients would necessitate more regular diagnostic testing and medication, thereby increasing these costs. CareMax's commitment to comprehensive care means maintaining a readily available stock of these vital resources, making it a recurring and essential expenditure.
Key cost drivers within this category include:
- Medical Supplies: Consumables such as gloves, masks, sterile dressings, and syringes.
- Diagnostic Equipment: Costs related to the purchase, maintenance, and calibration of equipment like EKGs, blood pressure monitors, and basic lab testing devices.
- Pharmaceuticals: Expenses for prescription medications and over-the-counter drugs dispensed to patients.
Marketing, Sales, and Patient Acquisition Costs
CareMax dedicates significant resources to marketing, sales, and patient acquisition, a key component of its cost structure. These costs are essential for attracting and enrolling new Medicare Advantage members and for nurturing ongoing relationships with health plans. In 2023, for instance, CareMax reported selling, general, and administrative expenses of $205.1 million, a substantial portion of which is allocated to these growth-driving activities.
These expenses encompass a variety of initiatives designed to reach potential patients and partners. This includes community outreach programs, targeted advertising campaigns, and the salaries of personnel focused on patient acquisition and retention.
- Marketing and Sales: Costs associated with advertising, community events, and promotional materials to attract Medicare Advantage members.
- Patient Acquisition Personnel: Salaries and benefits for staff directly involved in enrolling new patients and managing health plan relationships.
- Community Outreach: Expenses for local events, health fairs, and educational programs to build brand awareness and trust within target communities.
CareMax's cost structure is heavily influenced by its investment in medical and clinical staff, facility operations, and technology infrastructure. In 2023, selling, general, and administrative expenses, which include many of these costs, totaled $205.1 million.
The company also incurs substantial costs for patient care supplies and pharmaceuticals, directly linked to patient volume and treatment complexity. Marketing and patient acquisition efforts, including community outreach and advertising, represent another significant expenditure aimed at member growth.
| Cost Category | 2023 Expense (Millions USD) | Key Components |
|---|---|---|
| Selling, General & Administrative | $205.1 | Facility operations, marketing, sales, patient acquisition personnel, community outreach |
| Medical Supplies & Pharmaceuticals | (Not Separately Itemized) | Consumables, diagnostic equipment, prescription medications |
| Technology Infrastructure | (Included in SG&A/Operations) | Software development, data analytics, cybersecurity |
| Staff Salaries | (Substantial portion of operating costs) | Physicians, nurses, care coordinators |
Revenue Streams
CareMax's core revenue generation hinges on capitated payments from Medicare Advantage (MA) plans. This means they receive a set amount per member, per month, to oversee the complete healthcare of individuals enrolled in these plans.
This value-based approach, where they are paid to manage health rather than for individual services, strongly encourages a focus on preventative care and overall cost-effectiveness. For instance, in 2024, Medicare Advantage enrollment continued its upward trend, with projections indicating sustained growth, directly benefiting providers like CareMax who operate under this model.
CareMax heavily relies on performance-based bonuses and shared savings, a core component of its revenue. This model directly links financial gains to the company's success in meeting stringent quality metrics and cost-saving objectives within its value-based care agreements. For instance, in 2024, a substantial percentage of their revenue was anticipated to originate from these performance incentives, reflecting a commitment to patient well-being and operational efficiency.
While CareMax primarily focuses on value-based care, they do generate some fee-for-service revenue. This occurs for specific procedures or services not fully encompassed by their capitated agreements, or for patients not under their core value-based contracts. This supplemental income stream, though not central to their strategy, contributes to overall financial stability.
Other Healthcare Service Revenue
CareMax diversifies its income through various other healthcare services beyond primary care. These can include pharmacy operations within their centers, offering convenience to patients and generating revenue from prescription sales and associated services. Specialized health programs, like chronic disease management or wellness initiatives, also contribute to this revenue stream.
These ancillary services not only create additional income but also enhance the overall patient experience and reinforce CareMax's integrated care model. For instance, revenue can be generated from patient co-pays and deductibles for these specialized services, directly impacting the company's top line.
- Pharmacy Services: Revenue from prescription sales and over-the-counter medications.
- Specialized Programs: Income from disease management, wellness, and other targeted health initiatives.
- Patient Co-pays/Deductibles: Revenue collected from patients for specific services rendered.
Partnerships and Management Service Organization (MSO) Fees
CareMax generates revenue through strategic partnerships, acting as a Management Service Organization (MSO). This involves charging fees for the management services it provides to affiliated physician groups and other healthcare organizations.
Historically, CareMax has actively participated in MSO functions. They leverage their proven expertise in value-based care delivery and advanced technology to offer support and operational efficiencies to other providers in the healthcare ecosystem.
- MSO Fees: Revenue earned by providing management and administrative services to affiliated physician practices.
- Partnership Revenue: Income generated from collaborations with other healthcare entities, potentially including shared savings or service agreements.
- Value-Based Care Expertise: Monetizing their knowledge and systems for managing populations under value-based payment models.
- Technology Licensing/Support: Fees associated with providing access to or support for their proprietary technology platforms.
CareMax's revenue model is multifaceted, with capitated payments from Medicare Advantage plans forming the bedrock. This per-member, per-month payment structure incentivizes proactive health management. In 2024, Medicare Advantage enrollment continued its robust growth, directly benefiting CareMax’s strategy.
Performance-based bonuses and shared savings are critical revenue drivers, directly tying financial success to quality outcomes and cost efficiencies. These incentives represented a significant portion of their anticipated 2024 revenue, underscoring their commitment to value-based care principles.
Beyond core capitation, CareMax generates revenue from pharmacy services, offering prescriptions and over-the-counter items, and specialized health programs like chronic disease management. Patient co-pays and deductibles for these ancillary services also contribute to their income.
CareMax also functions as a Management Service Organization (MSO), earning fees for providing administrative and operational support to affiliated physician groups. This leverages their expertise in value-based care delivery and technology.
| Revenue Stream | Description | 2024 Relevance |
|---|---|---|
| Capitated Payments (MA) | Per-member, per-month payments for comprehensive healthcare management. | Primary revenue source, benefiting from continued MA enrollment growth. |
| Performance Bonuses/Shared Savings | Incentives tied to quality metrics and cost savings in value-based agreements. | Significant contributor, reflecting success in efficient patient care. |
| Pharmacy Services | Revenue from prescription sales and over-the-counter medications. | Diversifies income and enhances patient convenience. |
| Specialized Programs | Income from disease management, wellness, and targeted health initiatives. | Adds to revenue and reinforces integrated care model. |
| MSO Fees | Fees for management and administrative services to affiliated physician practices. | Monetizes expertise in value-based care operations. |
Business Model Canvas Data Sources
The CareMax Business Model Canvas is constructed using a blend of internal operational data, patient feedback, and healthcare industry market research. These sources provide a comprehensive view of our current performance and future opportunities.