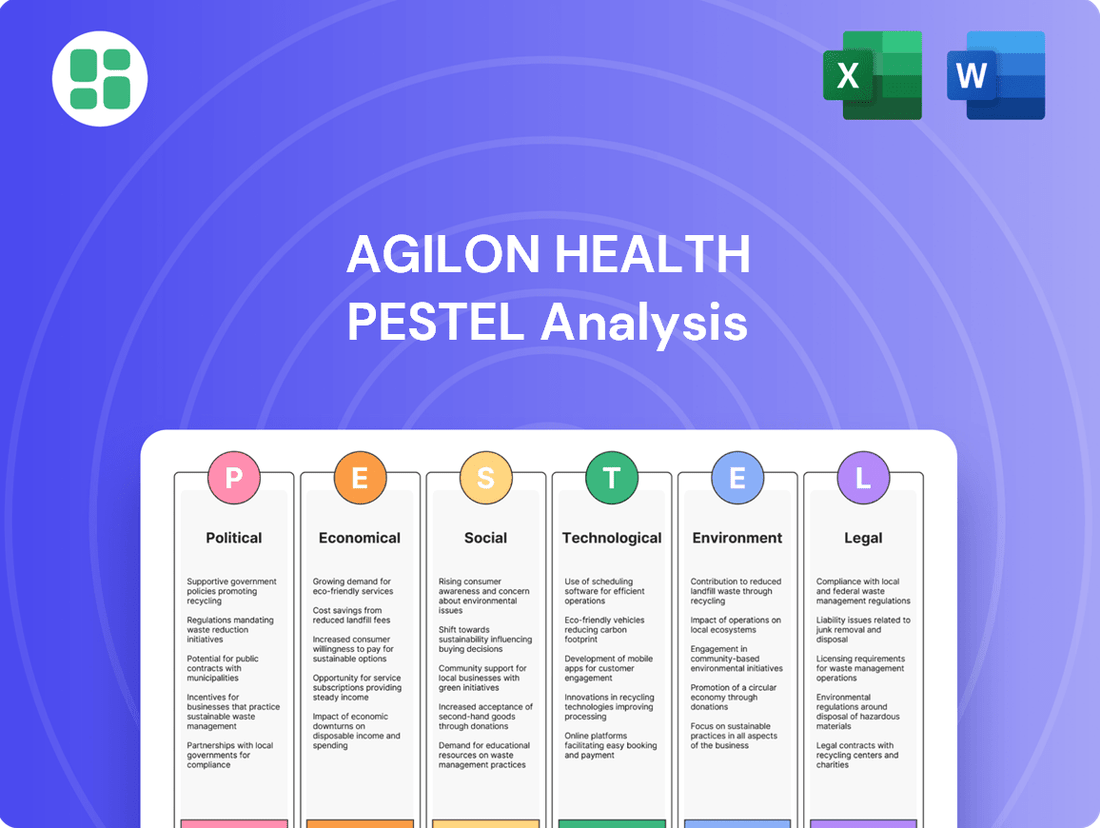
agilon health PESTLE Analysis
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
agilon health Bundle
Unlock the full picture of agilon health's operating environment with our comprehensive PESTLE analysis. Understand how political shifts, economic volatility, and evolving social trends are creating both opportunities and challenges for the company. This expert-crafted report provides the critical external intelligence you need to anticipate market changes and inform your strategic decisions. Download the complete PESTLE analysis now to gain a significant competitive advantage.
Political factors
The U.S. government, particularly through the Centers for Medicare & Medicaid Services (CMS), remains a significant driver for value-based care (VBC). This policy shift away from traditional fee-for-service reimbursement strongly aligns with and supports agilon health's core strategy of enabling physician groups to thrive in outcome-focused healthcare environments.
Initiatives like the Accountable Care Organization Realizing Equity, Access, and Community Health (ACO REACH) model exemplify this commitment. Discussions surrounding Medicare Advantage payment rates further underscore the sustained government focus on enhancing healthcare quality and controlling costs, especially within the senior population.
Medicare Advantage (MA) regulatory shifts are a critical political factor for agilon health. Changes in MA policies and payment rates directly affect the company's financial performance and operational strategies. For instance, proposed payment rate adjustments for contract year 2025, which consider risk score accuracy and medical cost trends, are closely watched by agilon health to project its revenue and medical margins.
agilon health actively participates in policy advocacy, submitting comments to the Centers for Medicare & Medicaid Services (CMS) on MA data and payment rate notices. This engagement aims to ensure that value-based primary care models receive appropriate funding, reflecting the evolving healthcare landscape and the company's commitment to improving patient outcomes.
The Inflation Reduction Act (IRA) introduces significant changes to healthcare costs, notably affecting Medicare Part D prescription drug benefits. This legislation directly impacts Medicare Advantage plans by capping out-of-pocket drug expenses for beneficiaries.
agilon health has proactively managed its exposure to these changes. For 2025, the company has strategically reduced its Part D membership to less than 30% of its total membership. This move is designed to mitigate potential financial headwinds stemming from the IRA's provisions on drug pricing and cost-sharing.
This strategic shift underscores agilon health's commitment to adapting to evolving federal healthcare legislation. By lowering its dependence on Part D revenue streams, the company is better positioned to navigate the financial implications of the IRA.
Anti-Fraud and Compliance Enforcement
The healthcare sector faces intense scrutiny from federal and state bodies concerning fraud, waste, and abuse. For agilon health, rigorous adherence to regulations, including those for Medicare and patient privacy, is paramount to prevent financial penalties from audits and protect its public image. In 2023, the U.S. Department of Justice announced resolutions in healthcare fraud cases totaling billions of dollars, underscoring the significant financial risks involved.
agilon health's commitment to compliance is a core element of its operational strategy. This focus helps mitigate risks associated with payor audits and ensures the company operates within legal frameworks, a critical factor given the industry's high regulatory burden.
- Regulatory Scrutiny: The healthcare industry is a prime target for anti-fraud and compliance enforcement actions.
- Financial Risk: Non-compliance can lead to substantial repayment obligations from payor audits, impacting profitability.
- Reputational Impact: Maintaining a strong compliance record is vital for safeguarding agilon health's reputation.
- Governance Emphasis: The company's governance framework prioritizes adherence to all relevant regulatory and legal mandates.
State-Level Healthcare Reforms
While Medicare is a federal program, state-level healthcare reforms significantly shape the operational landscape for agilon health's physician partners. These state-specific initiatives can range from adjustments in licensing requirements and scope of practice laws to the implementation of targeted programs designed to boost primary care accessibility or advance health equity.
For instance, states are increasingly exploring innovative payment models and care delivery pathways to manage costs and improve outcomes for their populations. Understanding and adapting to these diverse state regulatory environments is crucial for agilon health's strategic expansion and its ability to forge successful partnerships across various communities.
- State-specific reforms can impact physician reimbursement rates and patient eligibility for certain programs.
- Changes in scope of practice laws may allow for expanded roles for non-physician providers, influencing care team structures.
- States are actively pursuing initiatives to address social determinants of health, which can affect patient engagement and outcomes.
Government policy, particularly from CMS, strongly supports agilon health's value-based care model. Proposed Medicare Advantage payment rate adjustments for 2025 highlight the ongoing focus on quality and cost control. The company's strategic reduction of Part D membership to under 30% for 2025 mitigates IRA-related financial risks from prescription drug benefit changes.
agilon health actively engages in policy advocacy, submitting comments to CMS to ensure value-based primary care models receive adequate funding. The company's robust compliance framework is essential to navigate stringent regulations and avoid penalties, especially given the billions recovered in healthcare fraud cases in 2023.
State-level healthcare reforms also influence agilon health's operational environment, affecting physician partners through licensing, scope of practice, and new payment models. Adapting to these diverse state regulations is key for strategic growth and successful partnerships.
What is included in the product
This PESTLE analysis of agilon health examines how political, economic, social, technological, environmental, and legal factors create both challenges and opportunities for the company.
It provides a comprehensive view of the external landscape, offering actionable insights for strategic decision-making and competitive advantage.
The agilon health PESTLE analysis offers a streamlined, easily digestible summary of external factors, acting as a pain point reliever by simplifying complex market dynamics for quick referencing during strategic planning sessions.
Economic factors
agilon health continues to navigate elevated medical cost trends, a challenge that persisted through 2024 and is expected to carry into 2025, directly influencing its medical margin. The company observed a gross cost trend of 6.3% and a net trend of 5.3% in its year 2+ markets during the first quarter of 2025. This marks a slight decrease from the 7.1% gross cost trend reported in 2024, indicating some moderation but still requiring vigilant management.
These ongoing cost pressures underscore the critical need for agilon health to maintain and enhance its clinical and operational programs. Such initiatives are fundamental to effectively managing expenses, improving the predictability of its financial performance, and ultimately safeguarding its profitability in a dynamic healthcare landscape.
Changes in Medicare Advantage reimbursement, particularly the Centers for Medicare & Medicaid Services (CMS) risk adjustment model, have directly impacted agilon health. Lower-than-expected risk adjustment factors for 2024 and 2025 have created headwinds for the company.
This sensitivity was evident in agilon health's Q2 2025 results, where a negative medical margin was reported. A significant contributor to this was the reduction in risk adjustment revenue, underscoring the critical link between accurate risk scoring and financial performance in this sector.
agilon health's membership trajectory is a key economic driver, directly influenced by its Medicare Advantage and Accountable Care Organization (ACO) model participation. The company's strategic decisions in 2024 and 2025 to exit certain markets and partnerships have impacted its total member count. For instance, Q1 and Q2 2025 saw a reduction in platform members compared to prior periods due to these adjustments, a move intended to shed unprofitable exposure and enhance long-term financial health.
Despite these exits, agilon health secured new partnerships for the 2025 plan year, indicating continued expansion in select areas. This balancing act between market exits and new partner acquisitions highlights a strategic pivot towards optimizing profitability and ensuring growth is sustainable and performance-driven. The company's financial performance in 2025 will be closely scrutinized for the impact of these membership adjustments.
Capital Position and Profitability Path
agilon health's capital position remains robust, with substantial cash and marketable securities, providing a cushion during its current phase. However, recent financial performance, including net losses and negative Adjusted EBITDA, has prompted the suspension of their 2025 full-year guidance. This situation highlights a strategic pivot towards future profitability.
The company projects reaching break-even cash flow by 2027. This target is underpinned by their capital-light operational model and a concerted effort to enhance operational efficiency and financial transparency. The current period is characterized by necessary investments and restructuring to pave the way for sustained profitability.
- Capital Strength: agilon health reported approximately $740 million in cash and marketable securities as of the first quarter of 2024, demonstrating a strong liquidity position.
- Recent Financials: The company experienced net losses and negative Adjusted EBITDA in recent quarters, leading to a cautious outlook.
- Future Outlook: agilon health anticipates achieving break-even cash flow by 2027 through operational improvements and strategic initiatives.
- Guidance Suspension: Full-year 2025 guidance has been suspended, reflecting the ongoing adjustments and focus on achieving future financial stability.
Competitive Landscape and Payer Relationships
The economic viability of agilon health hinges on navigating a competitive value-based care landscape and fostering strong payer relationships. Securing favorable contracting terms, such as improved percentage of premium rates, directly impacts revenue yield and financial risk management. A key focus for agilon health is to reduce its exposure to Part D, a segment that has historically presented financial challenges.
agilon health's strategy involves actively refining its partnerships with health plans and optimizing the economic terms of these agreements. This proactive approach aims to bolster financial performance by ensuring contracts are structured to maximize revenue and minimize unmanaged risk. The company's success is directly tied to its ability to negotiate effectively with payers in an increasingly competitive market.
- agilon health's revenue yield is significantly influenced by payer contracting terms.
- Reducing Part D exposure is a strategic priority to mitigate financial risk.
- Optimizing percentage of premium rates is crucial for enhancing financial performance.
- The company is actively refining payer partnerships to improve contract economics.
Elevated medical cost trends, with gross cost trends at 6.3% and net trends at 5.3% in Q1 2025, continue to pressure agilon health's margins, though slightly down from 2024's 7.1% gross trend. Changes in Medicare Advantage reimbursement, specifically CMS risk adjustment factors, have created headwinds, contributing to a negative medical margin in Q2 2025 due to reduced risk adjustment revenue.
agilon health's membership has been impacted by strategic market exits in 2024 and 2025, leading to fewer platform members in Q1 and Q2 2025, but new partnerships secured for 2025 indicate a focus on optimizing profitability. The company's capital position remains strong with approximately $740 million in cash and marketable securities as of Q1 2024, but full-year 2025 guidance has been suspended due to recent net losses and negative Adjusted EBITDA.
The company aims to reach break-even cash flow by 2027, supported by its capital-light model and efficiency improvements, while also strategically reducing exposure to the financially challenging Part D segment and optimizing payer contract terms, such as percentage of premium rates.
| Metric | Q1 2024 | Q1 2025 | Q2 2025 |
|---|---|---|---|
| Gross Cost Trend | N/A | 6.3% | N/A |
| Net Cost Trend | N/A | 5.3% | N/A |
| Cash & Marketable Securities | ~$740 million | N/A | N/A |
What You See Is What You Get
agilon health PESTLE Analysis
The preview shown here is the exact document you’ll receive after purchase—fully formatted and ready to use. This comprehensive PESTLE analysis of agilon health delves into the Political, Economic, Social, Technological, Legal, and Environmental factors impacting the company's strategic landscape. Understand the external forces shaping agilon health's operations and future growth opportunities.
Sociological factors
The United States is experiencing a significant demographic shift with a rapidly aging population. In 2024, it's estimated that over 10,000 individuals turn 65 each day, a trend projected to continue and accelerate. This surge in seniors creates an ever-growing market for healthcare services specifically tailored to their needs.
This demographic wave directly impacts companies like agilon health, which focuses on value-based care. The increasing number of seniors, many with complex health needs and chronic conditions, drives demand for proactive and preventative healthcare solutions. By 2030, all baby boomers will be 65 or older, meaning 1 in 5 Americans will be retirement age, underscoring the long-term importance of this trend.
agilon health's model is designed to address these evolving senior healthcare needs. The company empowers physicians to manage the comprehensive health of these patients, emphasizing chronic disease management and preventative interventions. This approach aligns perfectly with the healthcare demands of an aging demographic, aiming for better outcomes and cost-effectiveness.
Senior patients increasingly favor healthcare that focuses on wellness and prevention, moving away from traditional reactive, fee-for-service models. This societal shift emphasizes a holistic approach to health, seeking integrated care rather than fragmented treatment.
agilon health's Total Care Model directly addresses this demand by prioritizing preventative measures and coordinated care teams. This strategy aims to enhance patient well-being and experience, aligning perfectly with the growing preference for proactive health management.
By focusing on prevention, agilon health's model is designed to reduce the incidence of costly hospitalizations and complex procedures. This not only benefits patient health but also contributes to a more sustainable healthcare system, a key consideration for an aging population.
Physician burnout, a significant challenge impacting primary care, is exacerbated by increasing administrative tasks. A 2024 survey indicated that over 60% of physicians report symptoms of burnout, often linked to EHR demands and regulatory compliance.
Many physicians express a strong desire for practice independence, seeking to escape the constraints of traditional employment models. This aspiration is driven by a wish to control patient care decisions and practice philosophy, a sentiment amplified by the administrative burdens they face.
agilon health's partnership model directly addresses these sociological factors by offering physicians the infrastructure, technology, and capital needed to operate independently within value-based care arrangements. This allows them to reduce administrative overhead and regain focus on patient well-being, thereby supporting the sustainability of the primary care workforce.
Health Equity and Access to Care
agilon health’s commitment to health equity and expanding access to primary care, especially in underserved regions, directly addresses a significant sociological concern. By focusing on vulnerable senior populations, the company aims to provide comprehensive care, thereby alleviating strain on existing healthcare infrastructure and channeling profits back into community health initiatives. This model fosters a healthier society by prioritizing those with the greatest need.
The company's efforts are particularly relevant given current healthcare disparities. For instance, in 2024, the Centers for Medicare & Medicaid Services (CMS) reported that rural Americans are more likely to be uninsured or underinsured compared to their urban counterparts, highlighting the critical need for agilon health's model. Their approach of partnering with local providers and investing in community-based care aims to bridge these access gaps.
Key aspects of agilon health's sociological impact include:
- Improving Health Equity: Directly tackles disparities by bringing quality primary care to areas with limited access.
- Supporting Vulnerable Populations: Focuses on senior patients, a demographic often facing complex health needs and access challenges.
- Community Reinvestment: Aims to reinvest profits into local healthcare resources, strengthening the community's overall health ecosystem.
- Reducing Healthcare Burden: By providing proactive and comprehensive care, agilon health seeks to lower emergency room visits and hospital readmissions, easing the load on public health systems.
Public Perception of Managed Healthcare
Public sentiment towards managed healthcare significantly impacts agilon health's operational landscape, affecting patient acquisition and physician engagement. Concerns regarding the industry's practices can create headwinds, potentially deterring both patients and healthcare providers.
agilon health actively addresses these perceptions by highlighting its physician-centric 'Total Care Model'. This approach, designed to support doctors in delivering patient-first, results-oriented care, is central to building confidence and cultivating a favorable public image.
The success of this strategy is partly reflected in patient satisfaction. For instance, in 2023, agilon health reported that 90% of its partner physicians' patients reported high satisfaction with their care, underscoring the positive reception of their model.
- Physician Trust: Public perception directly influences how readily physicians align with managed care organizations, impacting agilon health's network growth.
- Patient Enrollment: A positive view of managed care encourages patient enrollment, a critical factor for agilon health's revenue streams.
- Brand Reputation: Negative publicity surrounding managed care can tarnish the industry's image, necessitating proactive communication from companies like agilon health.
- Model Adoption: agilon health's emphasis on physician empowerment aims to counter negative stereotypes and foster trust in its unique approach.
The aging U.S. population, with over 10,000 individuals turning 65 daily in 2024, creates a substantial market for senior-focused healthcare. This demographic trend, projected to see all baby boomers aged 65+ by 2030, directly fuels demand for agilon health's value-based care model, which emphasizes proactive and chronic disease management for this growing segment.
Physician burnout, exacerbated by administrative burdens, with over 60% of physicians reporting burnout in a 2024 survey, drives a desire for practice independence. agilon health's model supports this by providing infrastructure and capital for physicians to operate independently within value-based care, reducing overhead and allowing a focus on patient care.
agilon health's commitment to health equity and access in underserved areas addresses significant sociological concerns, especially as rural Americans in 2024 were more likely to be uninsured. Their model of partnering with local providers and investing in community care aims to bridge these access gaps for vulnerable senior populations.
Public perception of managed healthcare influences patient and physician engagement. agilon health counters potential negative sentiment by promoting its physician-centric 'Total Care Model,' which in 2023 saw 90% patient satisfaction among partner physicians, highlighting the model's positive reception.
Technological factors
agilon health's commitment to advanced data visibility and analytics is a key technological driver. By leveraging sophisticated platforms, the company gains enhanced insights into both financial and clinical data. This is vital for accurately forecasting risk adjustment and medical cost trends, which directly impacts the financial health of their partnerships.
These technological capabilities are instrumental in identifying pathways to elevate the quality of care delivered by their physician partners. For instance, in 2024, agilon health continued to invest heavily in its data infrastructure, aiming to provide more granular performance metrics and predictive analytics to support value-based care initiatives. This focus on data-driven decision-making empowers physicians with actionable intelligence.
agilon health's core strength lies in its purpose-built platform, a critical technological enabler for value-based care. This platform provides physicians with the necessary technology, services, and capital to navigate the transition from fee-for-service to outcome-based reimbursement models.
The platform is designed to streamline operations, enhance care coordination, and ultimately improve patient outcomes. By centralizing these functions, agilon health empowers physician groups to focus on delivering quality care while managing the complexities of value-based contracts.
Continuous investment in platform enhancement is a key strategic imperative. In 2024, agilon health reported that its platform supported over 800,000 patients, demonstrating its scalability and impact. This ongoing development ensures the platform remains at the forefront of healthcare technology, driving greater efficiency and value for its partners.
The healthcare sector's embrace of telehealth and remote patient monitoring presents a significant technological factor for agilon health. By integrating these capabilities, agilon can bolster its patient-centered, preventative care model.
This integration promises to boost patient engagement and broaden access to healthcare services, especially for those managing chronic conditions. For instance, a report by Statista projected the global telehealth market to reach $191.2 billion by 2027, indicating substantial growth potential and a clear trend toward digital health solutions.
Cybersecurity and Data Privacy
Cybersecurity and data privacy are critical technological factors for agilon health, a company handling sensitive patient information. A data breach could result in substantial financial penalties and severe reputational damage, impacting customer trust and future growth. For instance, in 2023, the healthcare sector experienced a significant rise in cyberattacks, with the average cost of a data breach reaching $10.93 million, according to IBM's Cost of a Data Breach Report 2023. This underscores the immense financial risk associated with inadequate data protection measures.
agilon health's commitment to safeguarding patient data is not only an ethical imperative but also a legal necessity. The company must comply with stringent federal and state regulations, such as HIPAA (Health Insurance Portability and Accountability Act), which mandates strict standards for protecting patient health information. Failure to adhere to these regulations can lead to significant fines and legal repercussions. For example, HIPAA penalties can range from $100 to $50,000 per violation, with annual maximums reaching $1.5 million for repeat offenses.
The technological landscape is constantly evolving, requiring continuous investment in advanced cybersecurity solutions. This includes implementing multi-factor authentication, regular security audits, and employee training programs to mitigate risks. The increasing sophistication of cyber threats means that agilon health must remain vigilant and proactive in its defense strategies to protect its digital assets and patient data integrity.
Key considerations for agilon health in this area include:
- Robust Data Encryption: Implementing state-of-the-art encryption for data both in transit and at rest.
- Regular Security Audits: Conducting frequent vulnerability assessments and penetration testing to identify and address weaknesses.
- Employee Training: Providing ongoing education to staff on cybersecurity best practices and data privacy protocols.
- Compliance Management: Ensuring strict adherence to evolving data privacy regulations like HIPAA and state-specific laws.
AI and Machine Learning in Care Management
The integration of AI and machine learning into healthcare data analytics is a substantial technological avenue for agilon health. These advanced tools are instrumental in pinpointing patients who are most likely to experience adverse health events, thereby enabling proactive interventions.
Furthermore, AI can refine care delivery pathways, making them more efficient and effective, and also provide accurate predictions for future medical expenses. This predictive capability is crucial for managing costs within value-based care arrangements. For instance, by analyzing vast datasets, AI can identify patterns that lead to better resource allocation and cost containment.
By leveraging these innovations, agilon health can achieve significant reductions in the overall cost of care while simultaneously improving patient health outcomes. This technological edge is particularly valuable in their pursuit of success within value-based care models, where efficiency and effectiveness are paramount. Companies are investing heavily in this area; for example, the global AI in healthcare market was valued at approximately $15.4 billion in 2023 and is projected to grow substantially in the coming years, indicating a strong trend towards adoption.
Key applications of AI and ML for agilon health include:
- Predictive Analytics: Identifying patients at high risk of hospital readmission or chronic disease exacerbation.
- Care Pathway Optimization: Streamlining treatment plans and resource utilization for better patient journeys.
- Cost Forecasting: Accurately predicting healthcare expenditures to inform financial planning.
- Administrative Automation: Enhancing operational efficiencies through automated tasks and data processing.
agilon health's technological foundation centers on its proprietary platform, designed to facilitate value-based care by providing physicians with essential technology, services, and capital. This platform streamlines operations and enhances care coordination, with over 800,000 patients supported on the platform in 2024, showcasing its scalability.
The growing adoption of telehealth and remote patient monitoring, with the global telehealth market projected to reach $191.2 billion by 2027, offers agilon health opportunities to expand its patient-centered, preventative care model, boosting engagement and access.
Cybersecurity is paramount, given the sensitive patient data handled. The healthcare sector's average data breach cost reached $10.93 million in 2023, highlighting the financial and reputational risks. agilon health must adhere to regulations like HIPAA, where penalties can reach $1.5 million for repeat violations.
AI and machine learning are crucial for predictive analytics, identifying high-risk patients and optimizing care pathways. The global AI in healthcare market was valued at $15.4 billion in 2023, indicating significant investment and potential for cost reduction and improved outcomes.
Legal factors
agilon health navigates a complex web of Medicare and Medicaid regulations, crucial for its business model. Compliance with programs like Medicare Shared Savings Program (MSSP) and Accountable Care Organization Real Innovation Investment Model (ACO REACH) is paramount. For instance, in 2023, CMS reported over 1.2 million beneficiaries in ACO programs, highlighting the scale of these government-sponsored initiatives.
Failure to meet these stringent federal requirements, which cover everything from payment methodologies to quality metrics, can result in significant financial penalties and even exclusion from these vital government health programs. The Centers for Medicare & Medicaid Services (CMS) actively enforces these rules, making regulatory adherence a cornerstone of agilon health's operational strategy and financial health.
agilon health faces significant legal obligations concerning data privacy, particularly the protection of personally identifiable information and protected health information (PHI). This is a cornerstone of their operations, directly impacting patient trust and regulatory standing.
Compliance with the Health Insurance Portability and Accountability Act (HIPAA) and various state-level data privacy statutes is paramount. Failure to adhere to these regulations can result in substantial fines; for instance, HIPAA violations can lead to penalties ranging from $100 to $50,000 per violation, with annual maximums reaching $1.5 million per violation category, as of recent enforcement actions.
agilon health's corporate governance structure includes robust oversight mechanisms for patient confidentiality and privacy. This ensures that internal policies and practices align with legal mandates, safeguarding sensitive health data and reinforcing the company's commitment to ethical data handling.
agilon health operates within a healthcare landscape heavily influenced by federal anti-kickback statutes and Stark Law. These laws are designed to prevent financial relationships that could improperly influence patient referrals, meaning agilon's partnership structures must be meticulously crafted to avoid any appearance of illegal inducements. For instance, careful consideration is given to how payments are structured within their provider partnerships to ensure they reflect fair market value for services rendered, not compensation for patient volume.
Contractual Agreements with Physician Groups and Payers
agilon health's legal foundation is built upon its intricate contractual ties with physician groups and health plan payers. These agreements are the bedrock for risk-sharing models, defining how financial responsibilities are allocated and managed. For instance, the terms within these contracts dictate performance metrics and service standards, directly impacting patient care delivery and operational efficiency. In 2024, agilon health continued to emphasize the robustness and compliance of these agreements, recognizing their critical role in navigating the complex healthcare regulatory landscape.
The enforceability and clarity of these contracts are paramount for agilon health's financial health and operational continuity. They establish the parameters for data exchange, ensuring secure and compliant sharing of patient information, which is vital for coordinated care and value-based payment models. As of the first quarter of 2025, agilon health reported that the majority of its revenue was derived from these risk-based contracts, underscoring their significance to the company's business model.
- Contractual Framework: agilon health's business model hinges on legally sound contracts with physician groups and health plan payers.
- Risk-Sharing Arrangements: These agreements detail the financial risks and rewards associated with managing patient populations.
- Service Level Agreements (SLAs): Contracts specify performance benchmarks and quality metrics for healthcare services.
- Data Sharing Protocols: Legal stipulations govern the secure and compliant exchange of patient health information.
Antitrust and Market Consolidation Scrutiny
Antitrust regulators are increasingly scrutinizing consolidation within the healthcare sector, even for models focused on value-based care. While agilon health’s strategy centers on partnerships with physician groups rather than outright acquisitions, significant expansion or increased integration could still attract attention from bodies like the Federal Trade Commission (FTC). For instance, the FTC has been actively reviewing healthcare mergers and acquisitions, with a particular focus on those that could potentially reduce competition or increase costs for consumers.
Navigating this regulatory environment is crucial for agilon health's long-term growth. The company’s ability to forge new partnerships and deepen existing ones will be influenced by evolving antitrust interpretations. In 2024, the FTC continued its enforcement actions against healthcare deals, signaling a persistent focus on market competition.
- Increased regulatory scrutiny on healthcare partnerships and integrations.
- Potential for antitrust review even with a partnership-focused model.
- FTC's active role in monitoring healthcare market competition.
- Importance of strategic planning to address antitrust considerations for growth.
agilon health's legal framework is heavily shaped by government regulations, particularly those governing Medicare and Medicaid. Compliance with programs like the Medicare Shared Savings Program (MSSP) is essential, as demonstrated by the over 1.2 million beneficiaries in ACO programs reported by CMS in 2023. Adherence to quality metrics and payment rules is critical to avoid substantial penalties and maintain access to these vital government health programs.
Protecting patient data is a significant legal obligation, with HIPAA and state privacy laws dictating stringent requirements for handling protected health information (PHI). Violations can lead to severe fines, with HIPAA penalties potentially reaching $1.5 million per violation category annually. agilon health's corporate governance includes robust oversight to ensure alignment with these legal mandates and maintain patient trust.
The company's operations are underpinned by legally sound contracts with physician groups and health plans, which are crucial for its risk-sharing models. These agreements define financial responsibilities, performance standards, and data exchange protocols. As of Q1 2025, a significant portion of agilon health's revenue stemmed from these risk-based contracts, highlighting their critical importance.
Antitrust regulations pose a potential challenge, as regulators like the FTC are increasingly scrutinizing consolidation in healthcare. Even with a partnership-focused model, agilon health’s growth and integration strategies could attract attention, necessitating careful planning to address potential antitrust concerns. The FTC's continued focus on healthcare market competition in 2024 underscores this need.
Environmental factors
agilon health's commitment to ESG is evident in its Impact Report, showcasing a focus on sustainability and social responsibility. This proactive stance on non-financial performance signals a move towards holistic business evaluation, aligning with increasing investor demand for transparency in environmental and social impact.
The company's dedication to ESG reporting not only builds trust with stakeholders but also positions agilon health favorably within an investment landscape increasingly prioritizing sustainable and ethical business operations. This aligns with a broader trend where companies demonstrating strong ESG credentials often see improved access to capital and enhanced brand reputation.
agilon health's model is designed to positively impact community health by focusing on preventative care for senior patients, aiming to reduce hospitalizations. This approach directly lessens the strain on local healthcare resources, as fewer patients require acute, high-cost interventions. For instance, by keeping seniors healthier, the system can potentially lower readmission rates, a key metric for hospital efficiency.
The environmental benefit is realized through a more efficient healthcare delivery system. Less reliance on emergency room visits and inpatient stays translates to reduced consumption of resources like energy, water, and medical supplies within acute care facilities. This efficiency contributes to a more sustainable healthcare ecosystem.
Furthermore, agilon health's commitment to reinvesting shared profits into local primary care practices directly bolsters community health infrastructure. This reinvestment can fund enhanced services, improved technology, and better patient support programs, creating a stronger, more resilient primary care network within the communities it serves.
While agilon health's core business isn't directly tied to environmental management, climate change poses indirect challenges by shaping public health. For instance, rising global temperatures and increased frequency of extreme weather events, as highlighted by the World Health Organization's reports in 2024, can exacerbate respiratory illnesses and heat-related conditions.
These shifts can lead to a greater demand for healthcare services, potentially increasing medical costs and impacting the health outcomes of populations served by agilon health's partner physicians. The Centers for Disease Control and Prevention (CDC) noted in late 2024 that climate-sensitive diseases are showing concerning upward trends in certain regions, underscoring the need for adaptable healthcare strategies.
Sustainability in Healthcare Operations
While agilon health primarily operates as a technology and services platform, its role in influencing physician partners allows it to foster more sustainable healthcare operations. This influence can drive adoption of practices like energy efficiency and waste reduction across its network of clinics, contributing to a more environmentally conscious healthcare sector.
The company's platform can facilitate the implementation of greener initiatives, such as promoting energy-efficient lighting and HVAC systems in partner clinics. Furthermore, agilon health can encourage responsible procurement of medical supplies and equipment, prioritizing vendors with strong environmental, social, and governance (ESG) credentials.
- Energy Efficiency: Encouraging partner clinics to adopt LED lighting and smart thermostats, potentially reducing energy consumption by up to 20% in facilities.
- Waste Reduction: Promoting digital patient records and efficient supply chain management to minimize paper and medical waste, aiming for a 15% reduction in landfill-bound waste.
- Sustainable Procurement: Guiding physician partners to select suppliers with robust recycling programs and reduced packaging, impacting the environmental footprint of consumables.
Technological Carbon Footprint
Agilon health, as a technology-forward healthcare company, relies heavily on digital infrastructure, including data centers and cloud services. These operations inherently contribute to a carbon footprint, primarily through energy consumption. While the company's direct impact from healthcare delivery might be more substantial, the environmental cost of its technological backbone is an emerging area of focus for sustainability.
The company's commitment to efficiency in its digital operations, such as optimizing data storage and leveraging energy-efficient cloud providers, can significantly mitigate this footprint. For instance, many major cloud providers, which agilon health likely utilizes, are increasingly investing in renewable energy sources to power their data centers. In 2024, for example, major cloud providers aimed to power their operations with 75% renewable energy, a figure expected to climb higher in 2025.
- Data Center Energy Consumption: A significant portion of agilon health's technological carbon footprint stems from the energy required to power and cool its data centers and the servers supporting its digital platforms.
- Cloud Service Provider Initiatives: The company's reliance on cloud services means its environmental impact is also tied to the sustainability efforts of its providers, many of whom are committed to achieving net-zero emissions by 2030.
- Optimization Strategies: Implementing strategies like data deduplication, efficient coding practices, and choosing providers with strong green energy commitments can reduce the overall environmental impact of agilon health's technology stack.
Environmental factors influencing agilon health include the growing impact of climate change on public health, potentially increasing demand for healthcare services. The company's digital operations also contribute to a carbon footprint through energy consumption, though this can be mitigated by efficient practices and renewable energy investments by cloud providers.
PESTLE Analysis Data Sources
Our PESTLE Analysis for Agilon Health is built upon a robust foundation of data from official government health agencies, leading economic forecasting firms, and reputable industry associations. We incorporate insights from legislative updates, market research reports, and technological advancements impacting the healthcare sector.