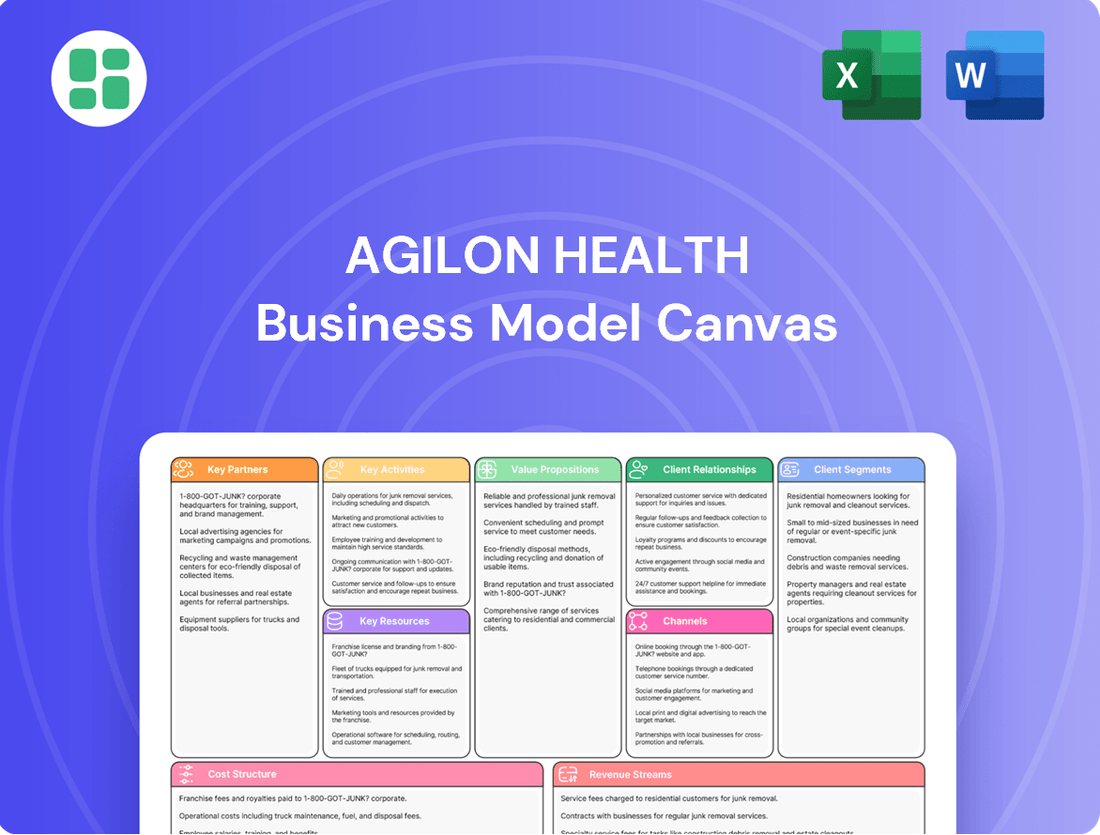
agilon health Business Model Canvas
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
agilon health Bundle
Unlock the strategic blueprint behind agilon health's innovative approach to value-based care. This comprehensive Business Model Canvas details how they partner with physicians, manage risk, and deliver superior patient outcomes. Discover the core elements driving their growth and market differentiation.
Ready to understand agilon health's competitive edge? Our full Business Model Canvas provides a deep dive into their customer relationships, revenue streams, and key resources. Download this actionable tool to gain insights for your own healthcare ventures.
Partnerships
Agilon Health’s core strategy hinges on deep, long-term alliances with independent primary care physician (PCP) groups. These partnerships are foundational, creating the essential network for delivering value-based care specifically to senior populations. In 2024, Agilon continued to expand its reach through these physician-led entities, aiming to improve patient outcomes and manage costs effectively within Medicare Advantage plans.
Agilon Health’s core strategy hinges on robust partnerships with health plans and payors, especially those focused on Medicare Advantage and Accountable Care Organization (ACO) frameworks. These collaborations are fundamental to implementing Agilon's global capitation and risk-sharing agreements, which are the bedrock of its value-based care model.
These payor relationships are critical for managing the financial aspects of care delivery and ensuring that incentives are aligned across the healthcare ecosystem. For instance, Agilon’s expansion into new markets often involves establishing these crucial payor agreements, allowing them to bring their model to more patients and providers.
In 2024, Agilon continued to deepen these relationships, aiming to expand its reach within the Medicare Advantage market. The success of these partnerships directly impacts Agilon's ability to generate revenue through capitation payments and manage the financial risks associated with patient populations.
Agilon Health partners with leading technology and data providers to bolster its platform. This strategic alliance involves leveraging robust cloud infrastructure, such as Microsoft Azure and Amazon Web Services (AWS), to ensure scalability and security for its extensive data operations.
By integrating advanced analytics and artificial intelligence tools from these partners, Agilon enhances its ability to aggregate and analyze vast amounts of health data. For instance, in 2024, Agilon continued to invest in these capabilities, aiming to refine its predictive models for patient outcomes and operational efficiency.
These collaborations are crucial for Agilon’s mission to deliver personalized care recommendations and improve health outcomes for seniors. The company's reliance on cutting-edge data processing and AI allows it to identify trends and provide actionable insights to its network of physicians.
Specialty Care Networks
Agilon Health’s model necessitates strong relationships with specialty care providers to offer comprehensive patient management, even though these aren't always formalized as traditional partnerships. Coordinating with specialists is crucial for the success of their Total Care Model, ensuring seniors receive all necessary medical attention.
This collaboration is key to improving patient outcomes and reducing costly hospitalizations by ensuring timely and appropriate specialist interventions. For instance, in 2024, Agilon continued to focus on integrating specialty care pathways to manage chronic conditions effectively.
- Specialist Coordination: Facilitating seamless referrals and communication between primary care physicians and specialists.
- Outcome Improvement: Working with specialists to reduce avoidable ER visits and hospital readmissions for common chronic diseases.
- Value-Based Care: Aligning specialist incentives with Agilon's overall goals for patient health and cost containment.
Community Organizations and Support Services
agilon health benefits from collaborations with community organizations and local support services to address social determinants of health for its senior patients. These partnerships are crucial for providing holistic care that extends beyond the doctor's office, focusing on improving overall patient well-being and fostering more patient-centered outcomes.
By integrating with these external entities, agilon health can offer a more comprehensive support system. This approach aligns with the growing understanding in value-based care that addressing factors like food security, transportation, and social isolation directly impacts health outcomes and reduces healthcare costs.
- Community Engagement: Partnering with local food banks, transportation services, and social programs helps seniors access essential resources.
- Improved Health Outcomes: Addressing non-medical needs often leads to better adherence to treatment plans and fewer hospital readmissions.
- Enhanced Patient Experience: Providing wrap-around services creates a more supportive and less stressful healthcare journey for seniors.
- Cost Efficiency: Proactive support in the community can prevent costly emergency room visits and hospitalizations.
Agilon Health's key partnerships extend to pharmaceutical companies and medical device manufacturers, ensuring its network has access to the latest treatments and technologies. These collaborations are vital for implementing evidence-based care protocols and managing medication costs effectively within its value-based frameworks.
In 2024, Agilon continued to refine its approach to these relationships, focusing on aligning incentives with providers to optimize the use of pharmaceuticals and medical supplies. This strategic alignment aims to improve patient adherence and reduce waste, contributing to overall cost savings and better health outcomes.
| Partner Type | Focus Area | 2024 Impact/Goal |
|---|---|---|
| PCP Groups | Value-based care delivery for seniors | Network expansion and improved patient outcomes |
| Health Plans/Payors | Medicare Advantage, ACOs | Capitation agreements, risk management |
| Tech/Data Providers | Cloud infrastructure, AI/Analytics | Scalability, data security, predictive modeling |
| Specialty Providers | Comprehensive patient management | Integrated care pathways, reduced hospitalizations |
| Community Organizations | Social determinants of health | Holistic patient support, improved well-being |
| Pharma/Device Companies | Latest treatments, cost management | Evidence-based protocols, optimized resource utilization |
What is included in the product
A comprehensive, pre-written business model tailored to agilon health's strategy of partnering with physician groups to improve value-based care outcomes.
Covers customer segments (physician groups, health plans), channels (direct sales, partnerships), and value propositions (improved patient outcomes, reduced costs) in full detail.
Agilon Health's Business Model Canvas acts as a pain point reliever by streamlining value propositions for providers and payers, offering a clear pathway to value-based care.
This canvas efficiently addresses the complexities of healthcare by mapping out key resources and activities that alleviate administrative burdens and improve patient outcomes.
Activities
A key activity for agilon health is actively guiding primary care physician groups through the complex transition from fee-for-service to value-based care arrangements. This involves a comprehensive support system designed to ease this shift.
agilon health provides essential tools, specialized training programs, and ongoing operational assistance to empower these physician groups. This hands-on approach ensures they have the resources needed to succeed in a risk-based environment.
The ultimate objective is to enable physicians to concentrate on improving patient outcomes and effectively managing the health of entire populations. For example, in 2024, agilon health reported that its partner physicians achieved significant improvements in key quality metrics, with a 15% reduction in hospital readmissions for their patient populations.
Agilon Health's core strength lies in its proprietary technology platform, which is constantly being updated and improved. This platform is essential for bringing together patient data, analyzing it, spotting areas where care is lacking, and helping doctors make better decisions.
In 2024, agilon health continued to invest heavily in its technology, particularly in artificial intelligence and advanced data analytics. These investments aim to sharpen their ability to predict health trends and refine their clinical programs, ensuring members receive the most effective care.
agilon health actively manages financial and risk exposure inherent in value-based care. This includes optimizing the economics of global capitation and shared savings agreements, a crucial element for sustained profitability in their model.
A significant focus is placed on mitigating risks associated with specific high-cost areas, such as Medicare Part D, and dynamically adjusting for evolving medical cost trends. This proactive approach ensures financial stability.
In 2024, agilon health demonstrated this by strategically exiting certain unprofitable partnerships, a move designed to sharpen their focus on profitable growth and reinforce their commitment to sound financial management.
Patient Population Health Management
Agilon Health actively manages the health of senior patient groups, especially those enrolled in Medicare Advantage and Accountable Care Organization (ACO) programs. This involves deploying clinical initiatives aimed at managing long-term illnesses, promoting preventive health measures, and initiating early treatments to boost patient well-being and lower overall healthcare expenditures.
The company’s focus on patient population health management directly contributes to better quality of care and improved patient outcomes. For instance, in 2023, agilon health reported that its partner physician groups achieved a 16% lower hospitalization rate for their Medicare Advantage patients compared to the national average, a testament to their proactive management strategies.
- Chronic Disease Management: Implementing tailored care plans for conditions like diabetes and heart disease.
- Preventative Care: Encouraging regular check-ups, screenings, and vaccinations.
- Early Intervention: Identifying at-risk patients and providing timely support to prevent escalation of health issues.
- Cost Reduction: Focusing on keeping patients healthy to minimize expensive hospitalizations and emergency room visits.
Network Expansion and Physician Onboarding
Agilon health actively pursues network expansion through new long-term partnerships with physician practices and health systems. This is a core activity to grow its reach and influence in value-based care.
The onboarding of new primary care physicians is a critical process, ensuring they are fully integrated into Agilon's platform and understand value-based care principles. This meticulous onboarding is key to successful adoption and patient outcomes.
- Network Growth: Agilon's strategy includes disciplined expansion within existing markets, aiming to deepen its penetration and impact.
- Physician Integration: Robust onboarding ensures new physicians can effectively leverage the Agilon platform for value-based care delivery.
- Partnership Development: Continuous formation of long-term partnerships with physician groups and health systems is fundamental to the business model.
agilon health's key activities revolve around enabling primary care physicians to thrive in value-based care models. This involves rigorous patient population health management, focusing on chronic disease management and preventative care to improve outcomes and reduce costs. For instance, in 2023, agilon health's partner physicians saw a 16% lower hospitalization rate for Medicare Advantage patients compared to the national average.
The company also actively manages financial risks inherent in these arrangements, optimizing capitation and shared savings agreements while strategically mitigating high-cost areas. This financial stewardship is crucial for long-term success. agilon health continues to invest in its proprietary technology platform, enhancing data analytics and AI capabilities to support clinical decision-making and predict health trends, as seen in their 2024 investments in these areas.
Furthermore, agilon health drives network expansion by forming new, long-term partnerships with physician practices and health systems, ensuring seamless integration and adherence to value-based care principles. This disciplined growth strategy aims to deepen market penetration and impact.
| Key Activity | Description | Impact/Data Point |
| Value-Based Care Transition Support | Guiding primary care physicians from fee-for-service to value-based care. | 15% reduction in hospital readmissions for partner physicians (2024). |
| Technology Platform Enhancement | Leveraging proprietary technology for data analysis and clinical decision support. | Continued heavy investment in AI and advanced data analytics (2024). |
| Population Health Management | Managing health of senior patient groups, focusing on chronic conditions and prevention. | 16% lower hospitalization rate for Medicare Advantage patients vs. national average (2023). |
| Financial Risk Management | Optimizing financial agreements and mitigating high-cost medical trends. | Strategic exit from unprofitable partnerships to focus on profitable growth (2024). |
| Network Expansion | Forming new long-term partnerships with physician practices and health systems. | Disciplined expansion within existing markets to deepen penetration. |
What You See Is What You Get
Business Model Canvas
The agilon health Business Model Canvas preview you're viewing is the actual document you will receive upon purchase. This means you're seeing the complete, unedited structure and content of the business model, ensuring full transparency. Once your order is processed, you'll gain immediate access to this exact file, ready for your strategic analysis and application.
Resources
Agilon Health's proprietary technology platform is a cornerstone of its business model. This cloud-based system is purpose-built to aggregate health data from a multitude of sources, offering sophisticated machine learning-infused analytics. For instance, in 2023, Agilon Health reported that its platform facilitated proactive recommendations for physicians, improving care coordination for its members.
The platform's ability to process and analyze vast amounts of patient health data is crucial for efficient management and informed decision-making. This advanced analytics capability allows Agilon Health to identify at-risk patients and recommend interventions, ultimately driving better health outcomes and cost savings. The company's focus on data-driven insights powered by this technology was a key driver in its strategy to manage capitated payments effectively.
Agilon health's physician network, boasting over 3,000 primary care physicians as of May 2024, is a cornerstone of its business model. This extensive network provides invaluable clinical expertise and deep, direct relationships with patients.
These physicians are not just participants; they are empowered by Agilon's platform, leveraging its tools and support to deliver enhanced care. This empowerment fosters a collaborative environment where best practices are shared, ultimately strengthening the entire network's capabilities and attractiveness.
Agilon Health's financial capital is a cornerstone of its business model, enabling it to provide crucial funding to physician groups. This capital injection helps these groups transition to value-based care, a key strategic initiative for the company.
As of March 2025, Agilon Health maintained a robust financial position with $369 million in cash. This liquidity is essential for funding ongoing operations, investing in critical technology advancements, and executing strategic growth plans.
Data Analytics and Medical Management Infrastructure
Agilon Health's core strength lies in its advanced data analytics and sophisticated medical management infrastructure. This allows them to process extensive health data, pinpointing individuals at higher risk and closely tracking performance metrics. These capabilities are fundamental to their population health management strategy, driving improved patient care and significant cost savings.
- Data Analytics & Engineering: Agilon leverages these to analyze vast datasets, enabling proactive interventions and personalized care plans.
- Medical Management Infrastructure: This robust system supports the monitoring of patient health, provider performance, and adherence to best practices.
- Population Health Management: The infrastructure is crucial for managing the health of entire patient populations, focusing on preventative care and chronic disease management.
- Performance Insights: Agilon's systems provide actionable insights that empower providers to enhance care quality and reduce healthcare expenditures.
Human Capital and Healthcare Expertise
Agilon Health's human capital is a cornerstone of its business model, particularly its deep expertise in healthcare operations, value-based care, and technology. This specialized knowledge is essential for building and refining their platform, fostering crucial partnerships, and expertly navigating the intricate landscape of healthcare regulations.
The company's workforce, encompassing its technology division, clinical professionals, and leadership team, collectively holds the necessary skills to drive Agilon's success in the value-based care sector.
As of December 31, 2024, Agilon Health reported a total of 1,076 employees, underscoring the significant human resources dedicated to its operations and strategic initiatives.
- Healthcare Operations Expertise: Staff possess in-depth knowledge of managing healthcare systems and patient care pathways.
- Value-Based Care Acumen: Employees are skilled in the principles and execution of value-based payment models.
- Technology Development: A dedicated technology team is vital for creating and enhancing the company's proprietary platform.
- Regulatory Navigation: The human capital is equipped to manage and comply with complex healthcare laws and policies.
Agilon Health's key resources are its proprietary technology platform, extensive physician network, financial capital, and specialized human capital. The platform's advanced analytics, as highlighted by its 2023 report on proactive physician recommendations, drives care coordination. The network, comprising over 3,000 primary care physicians as of May 2024, provides clinical expertise and patient relationships. Agilon's financial strength, evidenced by $369 million in cash as of March 2025, fuels its value-based care transition strategy. Finally, its human capital, with 1,076 employees as of December 31, 2024, brings essential healthcare operations, value-based care, and technology expertise.
| Resource Category | Key Components | Significance | Recent Data Point |
|---|---|---|---|
| Technology Platform | Proprietary cloud-based system, machine learning analytics | Enables data aggregation, proactive interventions, care coordination | Facilitated proactive recommendations for physicians (2023) |
| Physician Network | Over 3,000 primary care physicians | Provides clinical expertise, patient relationships, network growth | 3,000+ physicians (May 2024) |
| Financial Capital | Cash reserves, investment funding | Supports physician group transitions to value-based care | $369 million in cash (March 2025) |
| Human Capital | Healthcare operations, value-based care, technology expertise | Drives platform development, partnerships, regulatory navigation | 1,076 employees (December 31, 2024) |
Value Propositions
Agilon Health champions physician autonomy by equipping primary care providers with crucial insights, advanced tools, necessary capital, and performance-based incentives. This support system enables physicians to excel within value-based care models, preserving their independence and allowing them to prioritize patient well-being.
By alleviating administrative complexities and the traditional fee-for-service pressure to see more patients, agilon health allows physicians to concentrate on delivering quality care. For example, in 2024, agilon health supported over 2,500 physicians across various markets, demonstrating a tangible commitment to this physician-empowerment value proposition.
Agilon Health's model significantly enhances senior patient well-being through coordinated care, directly impacting health outcomes and creating a superior patient experience. This approach empowers physicians to prioritize holistic patient health, including proactive preventative measures and robust chronic disease management.
By shifting focus to total patient care, Agilon aims to reduce costly hospital admissions and emergency room visits. For instance, in 2024, Agilon reported that its partner physician groups achieved a 16% lower hospital admission rate compared to traditional Medicare fee-for-service models, demonstrating a tangible improvement in patient outcomes and a reduction in healthcare system strain.
Physician practices partnering with agilon health experience enhanced financial security and growth opportunities. This is achieved through participation in shared savings and global capitation models, directly benefiting doctors by aligning their incentives with improved quality outcomes and cost reduction.
In 2024, agilon health's physician partners demonstrated strong performance, with a significant portion achieving shared savings. For instance, in the first quarter of 2024, agilon health reported that its physician partners generated $150 million in shared savings, highlighting the financial upside of the model.
This approach fosters a sustainable business model for physicians by focusing on value-based care, which rewards efficiency and patient well-being over sheer volume of services. The emphasis on reducing waste and improving care coordination directly translates into better financial results for participating practices.
Reduced Healthcare Costs for Payors and System
agilon health's value-based care model is designed to significantly lower healthcare expenditures for both insurance providers (payors) and the broader healthcare system. By focusing on preventative care and proactive management of chronic conditions, the company aims to curb unnecessary medical services and hospital admissions.
This approach directly benefits payors by realigning their financial incentives. Instead of paying for the quantity of services rendered, they are compensated based on the quality of health outcomes achieved. This shift fosters more efficient healthcare spending and improved value for money.
For instance, agilon health reported that in 2023, its platform helped its partner physician groups achieve a 12% reduction in total medical expenses compared to traditional fee-for-service models. This translates to substantial savings for payors.
- Proactive Health Management: Reduces costs by preventing acute episodes and hospitalizations through continuous patient engagement and early intervention.
- Outcome-Based Reimbursement: Aligns financial incentives for providers with cost savings and improved patient health, benefiting payors.
- Reduced Unnecessary Services: Emphasizes evidence-based care and avoids costly, low-value treatments, leading to system-wide efficiency.
- Improved Chronic Disease Care: Better management of conditions like diabetes and heart disease lowers long-term healthcare costs and improves patient quality of life.
Access to a Peer Network and Best Practices
Agilon health's value proposition centers on providing physicians with unparalleled access to a robust peer network. This network comprises over 3,000 primary care physicians, creating a powerful collaborative environment.
This extensive network facilitates the sharing of vital clinical best practices and fosters a culture of innovation. Physicians can learn from each other's experiences, leading to continuous improvement in patient care delivery.
The network effect significantly enhances Agilon's platform appeal. It directly supports Agilon's mission to empower physicians and improve healthcare outcomes through shared knowledge and collective advancement.
- Physician Network Size: Over 3,000 primary care physicians.
- Key Benefit: Access to shared clinical best practices and collaborative innovation.
- Impact: Drives continuous improvement in care delivery and enhances platform value.
Agilon Health empowers physicians by providing them with the tools, capital, and performance incentives needed to thrive in value-based care, preserving their autonomy and focus on patient well-being. By reducing administrative burdens and fee-for-service pressures, Agilon allows over 2,500 physicians in 2024 to prioritize quality patient care and proactive health management.
The company enhances senior patient outcomes through coordinated care, enabling physicians to focus on holistic health, preventative measures, and chronic disease management. This focus leads to a 16% lower hospital admission rate for Agilon partner groups in 2024 compared to traditional Medicare, demonstrating improved patient health and reduced system strain.
Physician practices benefit from increased financial security and growth via shared savings and global capitation models, directly aligning incentives with quality and cost reduction. In Q1 2024 alone, Agilon partners generated $150 million in shared savings, showcasing the financial advantages of this value-based approach.
Agilon Health significantly lowers healthcare expenditures for payors and the system by emphasizing preventative care and chronic condition management, curbing unnecessary services. This model realigns payor incentives towards quality outcomes rather than service volume, fostering efficient spending.
| Value Proposition | Key Benefit | 2024 Data/Impact |
|---|---|---|
| Physician Autonomy & Empowerment | Tools, capital, incentives for value-based care | Supported over 2,500 physicians |
| Enhanced Patient Well-being | Coordinated care, proactive management | 16% lower hospital admission rate vs. FFS |
| Financial Security for Physicians | Shared savings, global capitation | $150 million shared savings (Q1 2024) |
| Reduced Healthcare Expenditures | Preventative care, chronic disease management | 12% reduction in total medical expenses (2023) |
Customer Relationships
Agilon Health fosters enduring partnerships with physician groups, typically committing to agreements that last up to 20 years. This long-term vision is built on a foundation of shared dedication to value-based care, where both parties are invested in achieving mutual success and improved patient outcomes.
This collaborative model provides physicians with ongoing support and resources, integrating them seamlessly into Agilon's operational framework. By empowering physicians, Agilon ensures they are well-equipped to navigate the complexities of value-based care, leading to enhanced patient satisfaction and financial performance.
agilon health prioritizes dedicated physician support, offering comprehensive onboarding and ongoing training to ensure seamless integration and effective platform utilization. This commitment is crucial for adopting value-based care principles.
The company actively engages in panel reviews and deploys targeted programs, such as those for high-risk patients, to minimize performance inconsistencies. In 2024, agilon health's platform supported over 1.2 million members, demonstrating the scale of their physician network engagement.
Agilon health cultivates strong customer relationships by delivering consistent, data-driven performance feedback directly to physicians. This approach, central to their platform, fosters collaboration aimed at enhancing both clinical outcomes and financial health for their partners.
The company's technology platform is key, offering physicians actionable insights and tailored recommendations. This transparency builds trust and supports a continuous improvement cycle in patient care delivery, a cornerstone of their relationship strategy.
For instance, in 2024, agilon health reported that its partner physicians, utilizing the platform's insights, saw an average improvement in quality scores. This data-driven feedback loop directly translates into better patient management and stronger financial performance for the physician groups.
Strategic Engagement with Health Plans
agilon health's relationships with health plans are deeply strategic, focusing on refining existing partnerships and negotiating contract terms. This ensures a mutual understanding and alignment on managing medical costs and designing benefits that truly serve members within a value-based care model. These ongoing dialogues are crucial for optimizing how risk is shared and ultimately improving both financial performance and patient health outcomes.
These engagements are not just transactional; they represent a collaborative effort to drive success in the value-based care landscape. By working closely with health plans, agilon health aims to create a sustainable ecosystem that rewards quality care and efficient resource utilization. For instance, in 2024, agilon health's partnerships are designed to incentivize proactive care management, which can lead to reduced hospitalizations and better chronic disease control.
- Partnership Refinement: Continuously improving collaboration with health plans to enhance operational efficiency and member satisfaction.
- Contract Negotiation: Securing mutually beneficial contract economics that support shared goals in cost management and quality improvement.
- Risk-Sharing Optimization: Structuring agreements to effectively share financial risk and reward, aligning incentives for better outcomes.
- Value-Based Care Alignment: Ensuring all aspects of the relationship support the transition to and success within value-based payment models.
Patient-Centered Care Coordination
Agilon health supports physicians in fostering patient-centered care coordination. While physicians maintain direct patient relationships, Agilon's platform and resources enable a more holistic approach to patient well-being, strengthening the doctor-patient bond.
By providing tools that streamline administrative tasks, Agilon empowers physicians to dedicate more quality time to each patient. This focus on the patient's total well-being is a cornerstone of their coordinated care model.
- Physician-Led Relationships: Doctors remain the primary point of contact and trust for patients.
- Agilon's Facilitation: The platform enables coordinated care, enhancing the physician's ability to manage patient health comprehensively.
- Increased Patient Focus: Tools provided by Agilon allow physicians to spend more time on patient needs and overall wellness.
- Reinforced Bonds: This enhanced physician attention cultivates stronger, more trusting patient relationships.
Agilon Health's customer relationships are built on deep, long-term partnerships with physician groups, often spanning up to two decades. This commitment is rooted in a shared focus on value-based care, ensuring mutual success and improved patient outcomes. In 2024, agilon health supported over 1.2 million members, highlighting the extensive reach of these physician relationships.
| Relationship Aspect | Description | 2024 Impact/Focus |
|---|---|---|
| Physician Engagement | Ongoing support, training, and data-driven feedback to empower physicians in value-based care. | Platform supported over 1.2 million members; partner physicians saw average quality score improvements. |
| Health Plan Collaboration | Strategic refinement of partnerships and contract negotiations to align on cost management and member benefits. | Focus on incentivizing proactive care management to reduce hospitalizations. |
| Patient-Centricity | Facilitating coordinated care that enhances the physician's ability to focus on patient well-being. | Tools designed to allow physicians more quality time with patients, strengthening doctor-patient bonds. |
Channels
Agilon Health actively pursues new physician partners through direct outreach, highlighting its Total Care Model and the advantages of value-based care. This strategy involves focused sales efforts and cultivating relationships with existing primary care practices and health systems.
In 2024, agilon health continued to expand its network, emphasizing the financial and clinical benefits its model offers to physicians. The company's direct engagement approach aims to onboard physician groups eager to transition to more patient-centric and outcome-driven care models.
Agilon health's proprietary technology platform is a cornerstone channel, directly connecting physician partners to the value Agilon provides. This digital interface is where doctors access crucial data analytics, streamline care coordination, and receive essential administrative support, all designed to enhance patient care and practice efficiency.
Physicians engage with Agilon's ecosystem through this sophisticated digital tool, which acts as a central hub for managing patient populations and accessing performance insights. For instance, in 2023, Agilon reported that its platform facilitated over 1.2 million patient encounters, highlighting the extensive use and integration of this technology in daily clinical workflows.
Agilon health's business model heavily relies on its on-site support and dedicated field teams. These teams are crucial for embedding Agilon's value-based care model directly within physician practices.
These field teams act as the hands-on facilitators, guiding practices through the complexities of value-based care transitions. They offer continuous operational assistance, ensuring that Agilon's proprietary processes and technology become seamlessly integrated into the everyday routines of healthcare providers.
For instance, Agilon's investment in these teams directly supports their mission to improve patient outcomes and reduce costs. In 2024, Agilon reported that its platform supported over 3,000 physicians across various markets, a testament to the reach and impact of its on-site support structure.
Industry Conferences and Thought Leadership
Agilon health actively participates in key healthcare industry conferences, such as the HLTH conference, to showcase its model and engage with potential partners. This presence helps raise awareness about their approach to value-based care. In 2023, Agilon reported a 26% increase in its partner network, highlighting the effectiveness of these outreach efforts.
Publishing research and engaging in thought leadership activities are crucial channels for Agilon. By sharing insights and data, they position themselves as innovators in the value-based care space. For instance, their white papers often detail the financial benefits and operational efficiencies achieved through their platform.
- Industry Conferences: Agilon's presence at events like HLTH and AHIP provides visibility and networking opportunities.
- Thought Leadership: Publishing research and participating in panels establishes Agilon as a leader in value-based care transformation.
- Partner Attraction: These channels are designed to attract new physician groups and health plans seeking to adopt a successful value-based care model.
- Brand Awareness: Consistent engagement in these forums reinforces Agilon's brand and its proven model's impact.
Investor Relations and Public Communications
agilon health leverages investor relations websites, annual reports, earnings calls, and press releases as key communication channels. These platforms are vital for delivering comprehensive financial data, strategic updates, and performance insights to its diverse stakeholder base. For instance, during their Q1 2024 earnings call, agilon health reported a revenue of $1.3 billion, demonstrating continued growth.
These channels are meticulously designed to cater to financially-literate decision-makers, offering transparency and detailed information. The company's investor relations website provides easy access to SEC filings, investor presentations, and historical financial performance, facilitating thorough analysis. In 2023, agilon health's total revenue reached $5.1 billion, up from $3.9 billion in 2022.
- Investor Relations Website: A central hub for financial reports, presentations, and company news.
- Annual Reports: Comprehensive documents detailing financial performance, strategic objectives, and market positioning.
- Earnings Calls: Live discussions providing real-time updates on financial results and management's outlook.
- Press Releases: Timely announcements of significant corporate developments and financial milestones.
Agilon Health's primary channels for physician engagement are direct outreach and its proprietary technology platform. These methods focus on demonstrating the tangible benefits of their value-based care model to healthcare providers.
On-site support teams are critical, acting as facilitators to integrate Agilon's processes into daily practice. Industry conferences and thought leadership activities further enhance brand awareness and attract new partners.
Investor relations and financial reporting channels are crucial for communicating performance and strategy to stakeholders. These platforms ensure transparency and provide data for informed decision-making.
| Channel | Description | Key Data/Impact |
|---|---|---|
| Direct Outreach & Sales | Targeted engagement with physician practices and health systems. | Focus on value-based care advantages. |
| Proprietary Technology Platform | Digital hub for data analytics, care coordination, and administrative support. | Facilitated over 1.2 million patient encounters in 2023. |
| On-Site Support & Field Teams | Embedding value-based care models and providing operational assistance. | Supported over 3,000 physicians across markets in 2024. |
| Industry Conferences & Thought Leadership | Showcasing the model and sharing insights to build brand and attract partners. | 26% increase in partner network in 2023. |
| Investor Relations & Financial Reporting | Communicating financial data, strategy, and performance to stakeholders. | Reported $1.3 billion revenue in Q1 2024; $5.1 billion total revenue in 2023. |
Customer Segments
Independent primary care physician groups are agilon health's foundational customer segment. These practices are actively looking to shift from the traditional fee-for-service payment system to value-based care arrangements.
These physician groups highly prioritize retaining their operational independence and physician autonomy. They seek a partner that can provide essential resources like capital, advanced technology platforms, and robust operational expertise to facilitate this transition.
In 2024, agilon health continued to serve a significant number of these physician groups, demonstrating their commitment to supporting independent physicians in the evolving healthcare landscape. Their model is designed to empower these groups by offering the necessary infrastructure to succeed under value-based care contracts.
Agilon Health partners with large health systems that have established primary care networks. These collaborations are designed to improve the financial and clinical performance of their Medicare Advantage patient populations under value-based care models.
These health systems are actively seeking ways to optimize their operations and patient outcomes. By integrating Agilon's platform and expertise, they aim to navigate the complexities of value-based reimbursement and achieve better results for both their patients and their bottom line.
For instance, in 2024, Agilon Health reported that its partner physician groups achieved significant improvements in key performance indicators. This includes a reduction in hospital admissions for their Medicare patients, a direct benefit of the enhanced care coordination facilitated by Agilon's model.
Senior patients, especially those in Medicare Advantage and Accountable Care Organization (ACO) programs, are the core focus of Agilon Health's value proposition. While they don't directly pay Agilon, their improved health and care experience are the ultimate goals. Agilon's model aims to deliver better health outcomes and more coordinated, accessible care for these individuals.
In 2024, Agilon Health's partner physician groups served approximately 1.2 million members, a significant portion of whom are seniors in Medicare Advantage plans. This vast patient base highlights the direct impact Agilon's integrated care model has on the daily lives and well-being of a substantial senior population, aiming to enhance their quality of life through proactive health management.
Health Plans and Government Payors
Health plans and government entities, such as the Centers for Medicare & Medicaid Services (CMS) through programs like ACO REACH, are key customers for Agilon Health. These organizations contract with Agilon's network of physician groups, viewing Agilon as a partner that helps them achieve critical objectives.
Agilon's model directly addresses their needs by focusing on reducing healthcare costs, enhancing the quality of care delivered, and improving the overall management of their member populations. For example, in 2024, Agilon's platform aims to deliver significant value to these payors by managing risk and improving outcomes for a growing number of patients.
These payors benefit from Agilon's ability to manage capitated payments effectively, driving better financial performance and patient satisfaction. Their engagement is crucial for the success of the value-based care model Agilon champions.
Key aspects of their customer relationship include:
- Cost Reduction: Payors contract with Agilon to lower overall healthcare expenditures for their covered members.
- Quality Improvement: They seek partners who can demonstrably improve patient outcomes and care coordination.
- Population Management: Agilon's model helps payors better manage the health of specific patient groups, particularly those in government programs.
- Value-Based Care Alignment: Health plans and government entities are increasingly shifting towards value-based reimbursement, making Agilon's approach a strategic fit.
Physicians Seeking Value-Based Care Expertise
Physicians increasingly frustrated with the limitations of the traditional fee-for-service system represent a key customer segment for agilon health. These providers are actively seeking a transition to value-based care but often find themselves without the essential infrastructure or specialized knowledge to navigate this shift effectively. Agilon offers a comprehensive solution tailored to empower these motivated physicians.
For these physicians, agilon health provides:
- Access to advanced analytics and care management tools designed to optimize patient outcomes and reduce costs.
- Expert guidance and support in navigating regulatory changes and implementing value-based payment models.
- A partnership that handles administrative burdens, allowing physicians to focus on patient care.
- Opportunities to participate in risk-sharing arrangements that reward quality and efficiency, a stark contrast to the volume-driven fee-for-service model.
agilon health's customer segments are diverse, encompassing independent primary care physician groups, large health systems, senior patients, and health plans/government entities. These groups are united by a shared interest in transitioning to value-based care models. In 2024, agilon health served approximately 1.2 million members, demonstrating its broad reach and impact on different stakeholders within the healthcare ecosystem.
| Customer Segment | Key Needs | agilon health's Offering | 2024 Relevance |
|---|---|---|---|
| Independent Primary Care Physician Groups | Transition to value-based care, retain independence, access to capital and technology | Platform, operational expertise, value-based care enablement | Continued partnership with numerous groups, facilitating their shift |
| Large Health Systems | Optimize financial/clinical performance, improve Medicare Advantage outcomes | Integration of platform and expertise for value-based care | Collaborations to enhance performance of primary care networks |
| Senior Patients (Medicare Advantage/ACO) | Improved health outcomes, coordinated care, accessible services | Enhanced care coordination and proactive health management | Direct beneficiaries of the model, impacting ~1.2 million members |
| Health Plans & Government Entities (e.g., CMS) | Cost reduction, quality improvement, population management | Risk management, value-based care partnership, improved financial performance | Key partners for achieving payor objectives in value-based care |
Cost Structure
The most significant part of agilon health's spending is on actual medical care for its members, covering things like doctor visits, hospital stays, and prescriptions. This is a direct reflection of the services they provide and is a key driver of their financial performance.
Agilon closely watches its Medical Margin, which is what's left after paying for all those medical services from the revenue generated. For instance, in the first quarter of 2024, agilon health reported a Medical Margin of $647 million, showcasing the substantial investment in patient care.
Agilon Health invests heavily in its proprietary technology platform, a core component of its business model. This includes ongoing development, enhancements, and maintenance of cloud services, data integration capabilities, and advanced AI and analytics tools. These investments are crucial for ensuring the platform remains robust, scalable, and capable of supporting Agilon's value-based care model.
In 2023, Agilon Health reported research and development expenses of $174.5 million. This significant outlay reflects the company's commitment to innovation and the continuous improvement of its technology infrastructure, which underpins its ability to manage and analyze patient data effectively.
Physician partner compensation, a significant cost driver, includes competitive base salaries and performance-based shared savings payments designed to align incentives. In 2024, Agilon health continued to invest in its physician network, with compensation structures directly tied to value-based care outcomes.
Beyond direct compensation, Agilon incurs substantial costs for onboarding new physician partners, providing comprehensive training on their platform and care models, and delivering ongoing operational support through dedicated teams. This investment ensures physicians can effectively transition to and thrive within Agilon's integrated system.
General and Administrative (G&A) Expenses
Agilon health's General and Administrative (G&A) expenses encompass the essential corporate overhead and salaries for its non-clinical workforce, covering critical functions like legal, finance, and overall operational management. These costs are fundamental to sustaining the company's infrastructure and strategic direction.
The company actively pursues enhanced operating expense efficiency, with a strategic aim to maintain platform support costs at a specific percentage of its revenue. This focus ensures that administrative functions contribute to, rather than detract from, overall profitability and scalability.
- Corporate Overhead: Costs associated with maintaining the central business operations and infrastructure.
- Non-Clinical Staff Salaries: Compensation for employees in administrative, legal, finance, and HR roles.
- Operational Expenses: Day-to-day costs necessary for running the business, excluding direct patient care.
- Efficiency Target: Platform support costs are managed as a percentage of revenue to optimize administrative spending.
Geographic Expansion and Market Entry Costs
Expanding into new geographies and establishing new partnerships involves significant market entry costs. These expenses are crucial for agilon health's strategy to scale its operations and build a presence in underserved communities.
While agilon health is pursuing a deliberate growth strategy, these costs represent an investment in future revenue streams and market share. For instance, in 2024, the company continued to focus on expanding its geographic footprint and deepening relationships with existing partners, which inherently involves upfront investment in sales, marketing, and operational setup in new regions.
- Market Entry Expenses: Costs associated with launching operations in new states or regions, including legal, regulatory, and initial staffing.
- Partnership Development: Investments in building relationships with new physician groups and healthcare providers, covering due diligence and onboarding.
- Sales and Marketing: Funds allocated to create awareness and attract new partners in target markets.
- Operational Setup: Expenses related to establishing local infrastructure and support systems for new partnerships.
The primary cost for agilon health centers on the direct medical care provided to its members, encompassing all aspects of healthcare delivery. This significant expenditure is directly tied to the company's core mission of managing patient health outcomes. Agilon's financial health is closely monitored through its Medical Margin, which in Q1 2024 stood at $647 million, illustrating the substantial resources allocated to member care.
Significant investments are also channeled into agilon's proprietary technology, including ongoing R&D, which totaled $174.5 million in 2023. This commitment fuels platform enhancements and data analytics capabilities essential for their value-based care model.
Physician compensation, a key cost, includes performance-based incentives aligned with value-based care outcomes. Furthermore, costs associated with onboarding new physician partners and providing ongoing support are substantial, ensuring effective integration into agilon's system.
General and Administrative (G&A) expenses, covering corporate overhead and non-clinical staff, are managed with an efficiency target for platform support costs relative to revenue. Market entry and partnership development also represent significant upfront investments for scaling operations into new geographies.
| Cost Category | Description | 2023 Data | 2024 Data (Q1) |
|---|---|---|---|
| Medical Care Costs | Direct expenses for patient health services | N/A | Reflected in $647M Medical Margin |
| Research & Development | Technology platform development and enhancements | $174.5 million | N/A |
| Physician Compensation | Salaries and performance-based incentives for physicians | N/A | Ongoing investment |
| General & Administrative | Corporate overhead and non-clinical staff costs | N/A | Managed for efficiency |
| Market Entry & Partnership | Costs for geographic expansion and new partner onboarding | N/A | Strategic investment |
Revenue Streams
Agilon Health's core revenue generation hinges on global capitation agreements. Under these arrangements, the company receives a predetermined monthly payment from health plans and other payors for each attributed Medicare patient. This payment is designed to cover the complete spectrum of healthcare services for those individuals, effectively transferring the financial risk associated with managing patient care from the payor to Agilon.
This model incentivizes Agilon to focus on value-based care, prioritizing patient outcomes and cost efficiency rather than the volume of services rendered. For instance, in 2023, Agilon reported that approximately 90% of its revenue was derived from these capitation arrangements, highlighting its central role in their financial strategy. This structure aligns Agilon's financial success with the health and well-being of its patient population.
Agilon Health's revenue model heavily relies on shared savings generated through value-based contracts. This means they earn money by improving patient health and lowering overall healthcare expenses, aligning their incentives with better care. For instance, in 2023, Agilon reported significant shared savings, contributing to their overall financial performance by demonstrating the effectiveness of their integrated care model.
For newer partnerships, especially those involving the 'Class of 2025' members, agilon health may initially recognize revenue through care coordination fees. This approach acts as a glide path, gradually transitioning towards full risk-sharing arrangements over time.
This initial fee structure provides a more predictable revenue stream for agilon health during the early stages of a partnership. For instance, in 2023, agilon health generated $1.3 billion in revenue, demonstrating its ability to scale its revenue models effectively.
Risk Adjustment Revenue
Agilon Health's revenue is significantly shaped by risk adjustment, a crucial element where payments are directly tied to the health status and overall complexity of the patient population they serve. This means that understanding and accurately representing the burden of illness within their patient groups is paramount for maximizing this revenue stream.
The company's financial performance in 2024 and leading up to mid-2025 relies heavily on the precision of their risk adjustment data submission processes. For instance, in their 2023 fiscal year, agilon health reported that risk adjustment revenue represented a substantial portion of their total revenue, underscoring its importance. The accuracy of their Hierarchical Condition Category (HCC) coding and the completeness of patient health records directly impact the capitation rates they receive from government programs like Medicare Advantage.
- Risk Adjustment Revenue: Payments are determined by the health status and complexity of the patient population.
- Data Accuracy is Key: Precise assessment and submission of patient health data are critical for optimizing this revenue.
- HCC Coding Impact: The accuracy of Hierarchical Condition Category coding directly influences capitation rates.
- 2023 Performance Indicator: Risk adjustment revenue constituted a significant portion of agilon health's total revenue in 2023, highlighting its financial importance.
Membership Growth and Expansion
Agilon health's revenue streams are significantly driven by membership growth. This growth encompasses both the increase in Medicare Advantage members and the overall expansion of the Agilon platform's member base. This expansion occurs through entering new geographic markets and deepening penetration within existing partner areas. For instance, in 2024, Agilon reported a substantial increase in its total membership, directly translating to higher revenue.
The company's financial performance is closely correlated with its ability to attract and retain members within its value-based care model. This organic and inorganic growth is the primary engine for increasing Agilon's top-line revenue.
- Membership Growth: Revenue directly scales with the number of Medicare Advantage members on the Agilon platform.
- Market Expansion: Entering new geographic markets contributes to a larger member base and thus increased revenue.
- Partner Growth: Deepening relationships and increasing member enrollment within existing partner geographies also fuels revenue.
- 2024 Performance: Agilon's reported membership figures for 2024 demonstrate a clear link between member acquisition and revenue generation.
Agilon Health's revenue is primarily generated through global capitation agreements, where they receive a fixed monthly payment per attributed Medicare patient from health plans. This model shifts financial risk to Agilon, incentivizing efficient, value-based care delivery. In 2023, approximately 90% of Agilon's revenue came from these capitation arrangements, underscoring their foundational role.
Shared savings from value-based contracts also contribute significantly, rewarding Agilon for improving patient health and reducing overall costs. This aligns their financial incentives with better patient outcomes. Agilon's 2023 performance highlighted substantial shared savings, validating their integrated care approach.
Risk adjustment is another critical revenue driver, with payments directly reflecting the health status and complexity of their patient population. Accurate Hierarchical Condition Category (HCC) coding and complete patient health records are vital for optimizing these payments from programs like Medicare Advantage. In 2023, risk adjustment represented a substantial portion of Agilon's total revenue.
Membership growth, encompassing both Medicare Advantage members and overall platform expansion, directly fuels revenue. This growth is achieved through new market entry and increased penetration in existing partner areas. Agilon's reported membership increases in 2024 directly correlated with higher revenue generation.
| Revenue Stream | Description | 2023 Significance | Key Driver |
|---|---|---|---|
| Global Capitation | Fixed monthly payments per attributed Medicare patient. | ~90% of 2023 Revenue | Patient Attribution & Health Status |
| Shared Savings | Earnings from improving patient health and lowering costs. | Contributed to financial performance | Value-Based Care Outcomes |
| Risk Adjustment | Payments based on patient health status and complexity. | Substantial portion of 2023 Revenue | HCC Coding Accuracy |
| Membership Growth | Revenue scales with the number of members on the platform. | Directly translated to higher revenue in 2024 | Market Expansion & Penetration |
Business Model Canvas Data Sources
The agilon health Business Model Canvas is constructed using a blend of internal financial data, comprehensive market research on healthcare trends, and insights derived from operational performance metrics. This multi-faceted approach ensures each component of the canvas is grounded in verifiable information.