Alignment Healthcare PESTLE Analysis
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
Alignment Healthcare Bundle
Gain an edge with our in-depth PESTEL Analysis—crafted specifically for Alignment Healthcare. Discover how political, economic, social, technological, legal, and environmental forces are shaping the company’s future, and use these insights to strengthen your own market strategy. Download the full version now and get actionable intelligence at your fingertips.
Political factors
Alignment Healthcare navigates the complex Medicare Advantage (MA) landscape, heavily influenced by the Centers for Medicare & Medicaid Services (CMS). The CMS final rule for 2025 MA plans, for instance, focuses on enhancing behavioral health access and standardizing broker payments, directly affecting operational strategies.
These regulatory shifts, including the review of utilization management for health equity, can significantly alter plan offerings and cost structures for Alignment Healthcare. For example, changes to prior authorization requirements could reduce administrative burdens or necessitate adjustments in provider network management.
The political climate significantly impacts Alignment Healthcare, particularly through potential healthcare reform initiatives. A shift in administration or congressional priorities could lead to changes in key programs like Medicare, Medicaid, and the Affordable Care Act. These changes might affect how Alignment Healthcare's Medicare Advantage (MA) plans are funded, structured, or who is eligible to enroll.
Alignment Healthcare's emphasis on value-based care models generally aligns with the direction many reforms aim to take. However, unforeseen legislative actions could present both new hurdles and avenues for growth. For instance, proposed changes to reimbursement rates for MA plans or new quality reporting requirements could directly influence profitability.
Looking at 2024, the political landscape remains dynamic. For example, discussions around Medicare Advantage growth and its cost-effectiveness continue. In 2023, Medicare Advantage enrollment surpassed 31 million beneficiaries, highlighting the program's significance. Any policy adjustments impacting this large enrollment base would naturally affect companies like Alignment Healthcare.
Alignment Healthcare faces significant political risk due to heightened regulatory scrutiny on Medicare Advantage plans. For instance, the Centers for Medicare & Medicaid Services (CMS) has intensified its oversight, including more frequent audits and stricter enforcement actions. This trend is evident in ongoing updates to processes like the appeals for Risk Adjustment Data Validation (RADV) audits, which directly impact revenue recognition for companies like Alignment.
Navigating this complex regulatory landscape requires Alignment Healthcare to maintain exceptionally robust compliance frameworks. Failure to adapt to evolving requirements, such as those related to coding accuracy and member eligibility, could lead to substantial financial penalties and damage to its reputation. The company's ability to proactively manage these political factors is crucial for its sustained operational and financial health.
Star Ratings and Quality Bonus Payments
Political factors significantly influence Alignment Healthcare through the Centers for Medicare & Medicaid Services (CMS) star rating system. This system directly links a plan’s performance to quality bonus payments and affects how many beneficiaries choose the plan. For instance, in 2024, plans achieving 4 or more stars can earn bonus payments, a critical revenue stream for companies like Alignment Healthcare.
Changes in how CMS calculates these star ratings, driven by political decisions, can create substantial financial volatility. A shift in methodology could alter Alignment Healthcare's bonus payment eligibility, impacting its profitability. The company's consistent achievement of high star ratings, often exceeding 4 stars across many of its plans, underscores the importance of this political landscape for its market standing and financial health.
- CMS Star Ratings: Medicare Advantage plans are evaluated on a 1-to-5-star scale, impacting bonus payments and member choice.
- Quality Bonus Payments: Higher star ratings directly translate to increased revenue for health insurers. In 2024, plans with 4+ stars are eligible for these bonuses.
- Political Influence: Changes in CMS rating methodologies, often politically driven, can significantly affect an insurer's financial performance and competitive advantage.
- Alignment Healthcare's Performance: The company's success in maintaining high star ratings is crucial for its financial stability and market position.
Lobbying and Advocacy Efforts
The healthcare sector, including Medicare Advantage (MA) organizations like Alignment Healthcare, actively engages in lobbying and advocacy to shape policy. These efforts aim to influence decisions concerning MA funding levels, regulatory frameworks, and the overall market structure. For instance, in 2023, the Medicare Advantage industry spent an estimated $130 million on lobbying efforts, seeking to protect payment rates and favorable regulations.
Alignment Healthcare, whether directly or through industry groups such as the Better Medicare Alliance, participates in these crucial discussions. Their advocacy can help to soften the impact of potentially unfavorable political shifts and cultivate an environment conducive to their business expansion and operational success.
- Lobbying Investment: The MA industry's significant lobbying expenditure in 2023 underscores its commitment to influencing policy.
- Policy Influence: Advocacy efforts focus on key areas like Medicare Advantage payment rates and regulatory oversight.
- Risk Mitigation: Effective lobbying can shield companies from adverse political changes and protect growth prospects.
- Industry Collaboration: Participation in industry associations amplifies the collective voice and impact of advocacy.
Political factors significantly shape Alignment Healthcare's operating environment through government regulations and policy decisions, particularly concerning Medicare Advantage (MA). The Centers for Medicare & Medicaid Services (CMS) dictates many aspects of MA plans, including reimbursement rates and quality standards.
For 2024, CMS finalized rules that impact MA plans, such as adjustments to the encounter data processing system and risk adjustment models, which directly influence revenue for companies like Alignment Healthcare. These regulatory shifts require continuous adaptation and robust compliance strategies.
The political landscape's influence extends to potential healthcare reforms, which could alter MA program funding, eligibility, or benefit structures. Alignment Healthcare's proactive engagement in policy discussions and advocacy efforts are crucial for navigating these political dynamics and safeguarding its business interests.
What is included in the product
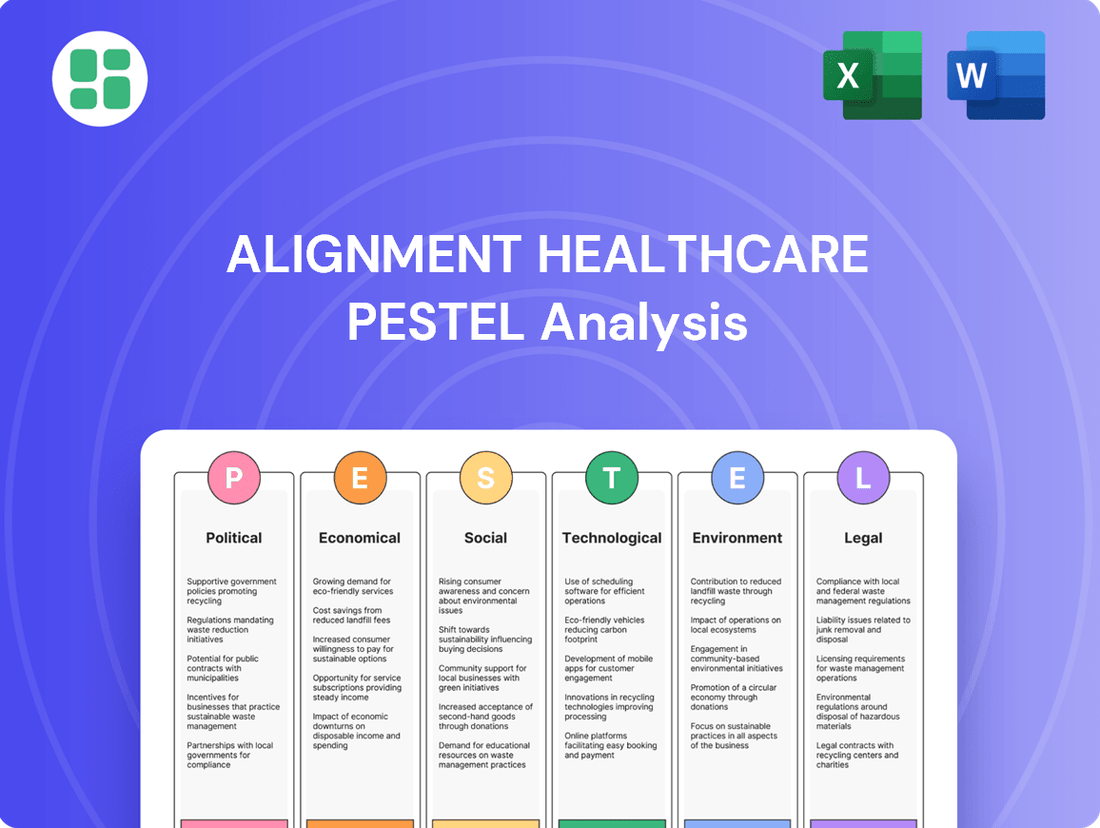
This PESTLE analysis provides a comprehensive examination of the external macro-environmental factors influencing Alignment Healthcare, covering Political, Economic, Social, Technological, Environmental, and Legal dimensions.
It offers actionable insights and forward-looking perspectives to empower strategic decision-making and identify potential opportunities and threats within the healthcare landscape.
Provides a concise version of Alignment Healthcare's PESTLE analysis that can be dropped into PowerPoints or used in group planning sessions, effectively relieving the pain point of time-consuming data synthesis.
Helps support discussions on external risk and market positioning for Alignment Healthcare by offering a clear PESTLE breakdown, alleviating the pain point of uncertainty in strategic decision-making.
Economic factors
Rising healthcare costs, driven by broader economic inflation, increased patient utilization, and the adoption of new medical technologies, pose a significant challenge to Alignment Healthcare's profitability. For instance, the U.S. experienced a 6.1% increase in medical care inflation in 2023, a rate that can outpace revenue growth.
As a Medicare Advantage provider, Alignment Healthcare operates within a fixed payment system, making it particularly susceptible to medical expense escalations that exceed their budgeted amounts. This fixed reimbursement model means that unexpected surges in healthcare utilization or treatment costs directly impact their bottom line.
To counter these pressures, Alignment Healthcare's success hinges on robust cost management. Implementing strategies like enhanced preventive care programs and effective chronic disease management can help control medical loss ratios. For example, investments in telehealth and remote patient monitoring, which saw significant growth in 2024, can lead to better patient outcomes and reduced overall healthcare spending.
The Centers for Medicare & Medicaid Services (CMS) sets the annual Medicare Advantage payment rates, which are a primary driver of Alignment Healthcare's revenue. For 2025, CMS projected an average payment rate increase of 3.3%. However, shifts in risk adjustment methodologies, like the move towards a V28 model, can significantly alter the actual reimbursement amounts plans receive.
These payment adjustments are critical for Alignment Healthcare's financial health, impacting its ability to manage costs and offer competitive benefits to its members. For instance, changes in risk scores can lead to variations in per-member, per-month payments, requiring robust financial modeling to anticipate and adapt to these fluctuations.
The Medicare Advantage landscape is a crowded space, featuring many large national insurers alongside smaller, regional competitors. This intense rivalry directly impacts pricing, as companies vie to offer attractive benefits and manage member acquisition costs effectively. For instance, in 2024, the Medicare Advantage market saw continued growth, with enrollment projected to reach over 30 million beneficiaries, highlighting the scale of competition.
Alignment Healthcare's strategy hinges on its distinct 'high-tech, high-touch' approach, which emphasizes personalized care and a technology-driven member experience. This differentiation is crucial for standing out amidst a field where many providers offer similar core benefits. The company’s ability to execute this model efficiently will be key to its economic success in attracting and retaining members in this highly competitive environment.
Senior Disposable Income and Cost-Sharing
Senior disposable income is a critical factor influencing healthcare choices, including enrollment in Medicare Advantage plans offered by companies like Alignment Healthcare. While these plans often aim to lower out-of-pocket expenses, the actual ability of seniors to manage cost-sharing, such as copayments and deductibles, remains paramount. Economic conditions directly impact this disposable income, making beneficiaries more discerning about plan costs.
Rising inflation and the general cost of living can significantly erode the purchasing power of seniors. For instance, if the Consumer Price Index (CPI) continues its upward trend, as seen in recent years, the real value of fixed incomes diminishes, making even modest premiums and deductibles a greater burden. This sensitivity can lead to shifts in enrollment patterns, favoring plans with lower upfront costs or more predictable expenses.
- Impact of Inflation: Persistent inflation can reduce the real value of Social Security benefits and other retirement income, directly affecting seniors' disposable income. For example, a 3% inflation rate on a $2,000 monthly retirement income effectively reduces purchasing power by $60 per month.
- Cost-Sharing Sensitivity: As out-of-pocket healthcare costs increase, seniors with less disposable income may delay or forgo necessary medical services, impacting their health outcomes and satisfaction with their insurance plans.
- Plan Selection Dynamics: Economic pressures can drive seniors towards Medicare Advantage plans with lower monthly premiums, even if those plans involve higher copays for certain services, reflecting a trade-off based on immediate affordability.
Investment Climate and Capital Access
Alignment Healthcare's ability to access capital is directly tied to the prevailing investment climate and interest rate environment. Favorable conditions, characterized by low interest rates and investor confidence, enable the company to pursue growth strategies and fund new initiatives more readily. Conversely, a tightening credit market or increased investor risk aversion can constrain its expansion capabilities.
The company's recent financial performance, including positive earnings reports and consistent membership growth, underscores a robust financial footing. For instance, Alignment Healthcare reported a net income of $101.5 million for the first quarter of 2024, a significant increase from the previous year, signaling strong operational execution and market demand. This financial strength enhances its attractiveness to investors and improves access to capital markets for future investments.
Key factors influencing Alignment Healthcare's investment climate and capital access include:
- Interest Rate Environment: Fluctuations in interest rates directly impact the cost of borrowing for expansion and operational financing. Lower rates in 2023 and early 2024 generally supported easier capital access.
- Investor Sentiment: Positive market sentiment towards healthcare providers and managed care organizations, driven by factors like favorable regulatory outlooks and demographic trends, boosts investor confidence and capital availability.
- Company Performance: Strong revenue growth, as seen with Alignment Healthcare's 2023 revenue of $1.7 billion, up from $1.3 billion in 2022, directly correlates with improved access to capital by demonstrating financial health and growth potential.
- Market Liquidity: The overall liquidity in capital markets affects the ease with which companies can issue debt or equity. A liquid market generally translates to better terms and broader access for companies like Alignment Healthcare.
Economic factors significantly influence Alignment Healthcare's operational environment. Rising healthcare costs, exacerbated by inflation, directly challenge profitability, especially given the fixed reimbursement rates of Medicare Advantage plans. For example, while CMS projected a 3.3% payment rate increase for Medicare Advantage in 2025, this must be weighed against medical cost inflation, which saw medical care inflation at 6.1% in 2023.
Senior disposable income is a crucial determinant of plan selection. Economic pressures can make cost-sharing components like copayments more burdensome, potentially leading seniors to prioritize lower premium plans. For instance, persistent inflation erodes the purchasing power of fixed retirement incomes, making even modest out-of-pocket expenses a greater concern for beneficiaries.
Alignment Healthcare's access to capital is tied to the broader investment climate and its own financial performance. Strong revenue growth, such as Alignment Healthcare's revenue of $1.7 billion in 2023 (up from $1.3 billion in 2022), coupled with positive net income of $101.5 million in Q1 2024, enhances its ability to secure funding for growth initiatives.
What You See Is What You Get
Alignment Healthcare PESTLE Analysis
The preview shown here is the exact document you’ll receive after purchase—fully formatted and ready to use. This comprehensive PESTLE analysis of Alignment Healthcare delves into the Political, Economic, Social, Technological, Legal, and Environmental factors impacting the company's operations and strategic direction. Understand the external forces shaping the healthcare landscape and Alignment Healthcare's position within it.
Sociological factors
The United States is experiencing a significant demographic shift with a rapidly growing senior population. By 2030, an estimated 73 million Americans will be 65 or older, a substantial increase from today. This trend directly fuels demand for healthcare services tailored to older adults, making it a key sociological factor for companies like Alignment Healthcare.
As the number of seniors escalates, so does the need for Medicare Advantage plans, which are designed to cover the healthcare needs of this demographic. Alignment Healthcare, with its focus on serving seniors, is well-positioned to capitalize on this expanding market. The company's offerings, including specialized care and health plan options, align directly with the increasing healthcare requirements of this aging population.
There's a clear societal shift, especially among older adults, towards healthcare that feels tailored and works seamlessly. They want convenience and a more personal touch in how they receive care.
Alignment Healthcare's approach, which combines advanced technology with human interaction through local care teams and coordinated support, perfectly matches this growing preference. This focus on preventive care and integrated services resonates strongly with what consumers are looking for in 2024 and beyond.
By aligning with these consumer desires, Alignment Healthcare is well-positioned to boost member satisfaction and loyalty. For instance, a 2024 survey indicated that 78% of seniors prioritize personalized communication from their healthcare providers, a key element of Alignment's strategy.
Societal awareness regarding preventive healthcare and chronic disease management is on the rise, a trend that directly benefits Alignment Healthcare's business model. As more seniors and their families actively participate in health management, the demand for health plans emphasizing preventive services and comprehensive chronic condition support is increasing. This growing engagement is projected to improve overall health outcomes and potentially reduce long-term healthcare expenditures, aligning perfectly with Alignment Healthcare's value proposition.
Social Determinants of Health
There's a growing understanding that factors outside of traditional medical care significantly influence health outcomes. Things like having enough healthy food, stable housing, and reliable transportation are now recognized as crucial social determinants of health (SDOH). This societal shift is prompting healthcare providers to think more broadly about member well-being.
Alignment Healthcare is actively engaging with this trend. Their involvement in programs like the Centers for Medicare & Medicaid Services (CMS) Value-Based Insurance Design (VBID) Model is a prime example. This model specifically allows for supplemental benefits that address SDOH, directly aligning with the recognized importance of these social factors.
By focusing on SDOH, Alignment Healthcare aims to improve health equity and enhance the overall well-being of their members. For instance, in 2024, the VBID model continued to explore innovative ways to integrate SDOH interventions into Medicare Advantage plans, with a focus on reducing healthcare costs and improving member satisfaction.
- Growing SDOH Awareness: Societal recognition of food, housing, and transportation as key health drivers is increasing.
- VBID Model Participation: Alignment Healthcare's engagement in CMS's VBID Model directly supports SDOH interventions.
- Health Equity Focus: Addressing SDOH is central to improving fairness and outcomes across diverse member populations.
- Member Well-being Enhancement: Proactive support for social needs contributes to better overall health and quality of life for members.
Caregiver Burden and Support Needs
The growing number of individuals requiring care, often due to an aging population, places a significant and increasing burden on family caregivers. This societal trend underscores a critical demand for accessible and effective support services. For instance, in the US, an estimated 53 million adults provided unpaid care in the past year, a number projected to rise. Alignment Healthcare is addressing this by expanding caregiver benefit access and implementing programs such as 'Care Anywhere,' which aims to provide more flexible and home-based care solutions.
By offering robust resources and support systems for these caregivers, companies like Alignment Healthcare can significantly improve member satisfaction and streamline the overall care coordination process. This not only benefits the individuals receiving care but also strengthens the healthcare provider's relationship with its members and their families. A 2024 AARP report indicated that caregivers often experience high levels of stress, making targeted support crucial for their well-being and the quality of care they provide.
- Societal Shift: An aging demographic is increasing the demand for caregiving, placing a greater strain on family members.
- Alignment Healthcare's Response: The company is enhancing caregiver benefits and introducing programs like 'Care Anywhere' to meet these evolving needs.
- Impact of Support: Providing resources for caregivers can lead to improved member satisfaction and more efficient care coordination.
- Data Point: Over 53 million adults in the US acted as unpaid caregivers in the past year, highlighting the scale of this societal factor.
The increasing recognition of social determinants of health (SDOH) is a significant sociological factor. Alignment Healthcare's participation in the CMS Value-Based Insurance Design (VBID) Model demonstrates a commitment to addressing these non-medical needs, such as food security and housing stability, which directly impacts member well-being and health outcomes.
The growing burden on family caregivers is another key sociological trend. With an estimated 53 million unpaid caregivers in the US in the past year, Alignment Healthcare's expansion of caregiver benefits and programs like 'Care Anywhere' addresses this critical need, aiming to improve member satisfaction and care coordination.
Societal preferences are shifting towards personalized and convenient healthcare experiences, particularly among seniors. Alignment Healthcare's strategy, combining technology with local care teams, directly caters to this demand for tailored, human-centric care, a trend reinforced by 2024 data showing 78% of seniors prioritizing personalized communication.
The aging demographic in the United States, with 73 million individuals expected to be 65 or older by 2030, fundamentally drives demand for senior-focused healthcare services. Alignment Healthcare is strategically positioned to benefit from this demographic shift, as the need for Medicare Advantage plans and specialized senior care continues to rise.
Technological factors
Alignment Healthcare's competitive advantage is significantly bolstered by its proprietary AI-powered AVA platform. This technology is central to its strategy of delivering personalized care and proactively managing patient health outcomes. For instance, AVA's capabilities are designed to identify at-risk members, enabling early intervention and thereby reducing the incidence of high-cost care events.
The AVA platform's ability to predict health risks and optimize care delivery is a key differentiator. By analyzing vast amounts of patient data, AVA helps clinicians make more informed decisions, leading to better patient results and more efficient resource allocation. This focus on data-driven insights is crucial in the evolving healthcare landscape.
Continued investment in and ongoing enhancement of platforms like AVA are paramount for Alignment Healthcare to maintain its leading position. As of their latest reports, the company emphasizes the ongoing development of these technological assets to further refine their care management solutions and expand their market reach.
The swift evolution and widespread acceptance of telehealth and remote monitoring are directly impacting Alignment Healthcare's 'Care Anywhere' initiative. These innovations facilitate virtual doctor visits, at-home patient monitoring, and remote health tracking, significantly boosting accessibility and ease of use for elderly individuals, particularly those facing mobility challenges.
By leveraging these technological strides, Alignment Healthcare can enhance patient engagement and streamline care delivery. For instance, the global telehealth market was projected to reach over $500 billion by 2027, indicating a substantial and growing infrastructure for such services in the 2024-2025 period.
Alignment Healthcare's core strategy hinges on sophisticated data analytics and predictive modeling. By processing vast amounts of health data, the company can pinpoint members at higher risk for adverse health events, enabling proactive interventions. This data-driven approach is crucial for tailoring care plans and optimizing the deployment of their care coordination resources, directly impacting patient outcomes and cost management.
The company's investment in data science is not just about current operations; it's a commitment to future innovation. For instance, advancements in AI and machine learning are continuously refining their ability to forecast health trends and personalize treatment pathways. This ongoing evolution in analytical capabilities is vital for maintaining a competitive edge and enhancing the effectiveness of their integrated care model.
Cybersecurity and Data Privacy
Cybersecurity and data privacy are critical for Alignment Healthcare, given its handling of sensitive patient health information. Maintaining robust defenses against data breaches and ensuring strict adherence to regulations like HIPAA is non-negotiable for preserving patient trust and avoiding significant legal penalties. The company's ongoing investment in secure IT infrastructure directly supports these efforts, reflecting the high stakes involved in protecting personal data.
The healthcare industry, in general, faces escalating cyber threats. For instance, in 2023, the U.S. Department of Health and Human Services reported over 133 million healthcare records were compromised in breaches affecting 655 healthcare organizations. This underscores the constant need for vigilance and advanced security measures within companies like Alignment Healthcare.
- Data Breach Costs: The average cost of a healthcare data breach in 2023 reached $10.93 million, a significant increase from previous years.
- HIPAA Fines: Non-compliance with HIPAA can result in substantial fines, with penalties ranging from $100 to $50,000 per violation, capped at $1.5 million per year for repeat offenses.
- Patient Trust: A single significant data breach can erode patient confidence, impacting customer retention and brand reputation.
- Regulatory Scrutiny: Increased regulatory focus on data privacy means companies must proactively demonstrate compliance to avoid investigations and sanctions.
Interoperability and Health Information Exchange
The ability for Alignment Healthcare to seamlessly share patient data with its network of doctors, hospitals, and other healthcare providers is vital for delivering coordinated care. This interoperability is becoming increasingly important as the healthcare landscape moves towards more integrated models. For instance, the U.S. Department of Health and Human Services has been pushing for greater health information exchange, with initiatives aimed at improving data sharing capabilities. By 2024, it's estimated that over 90% of hospitals in the U.S. were participating in health information exchanges, highlighting the growing trend towards connected care systems.
Improvements in interoperability standards, such as FHIR (Fast Healthcare Interoperability Resources), and better integration with electronic health records (EHRs) directly benefit Alignment Healthcare. These advancements can significantly boost care coordination, allowing for quicker access to patient histories and treatment plans. This efficiency can lead to better patient outcomes and reduce the likelihood of duplicate testing or medication errors. In 2023, studies indicated that healthcare organizations with strong interoperability reported higher levels of patient satisfaction and improved operational efficiency.
- Interoperability Standards: Advancements in FHIR APIs are facilitating easier data exchange between disparate healthcare systems.
- EHR Integration: Enhanced EHR integration allows for a more unified view of patient health information across Alignment Healthcare’s network.
- Care Coordination: Seamless data flow improves the ability of physicians and hospitals to coordinate treatment plans effectively.
- Efficiency Gains: Streamlined information exchange can reduce administrative burdens and operational costs within the healthcare ecosystem.
Alignment Healthcare's technological edge is powered by its proprietary AI platform, AVA, which personalizes care and identifies at-risk members for early intervention. This data-driven approach optimizes care delivery and resource allocation, a critical factor in the evolving healthcare landscape.
The company's commitment to enhancing AVA and other technological assets is key to maintaining its market position, with ongoing development focused on refining care management solutions and expanding reach. Telehealth and remote monitoring innovations, like those supporting Alignment's Care Anywhere initiative, are significantly boosting accessibility, especially for elderly individuals.
The global telehealth market's projected growth, potentially exceeding $500 billion by 2027, highlights the robust infrastructure supporting these virtual services through 2024-2025. Advanced data analytics and predictive modeling are central to Alignment's strategy, enabling proactive interventions by pinpointing members at higher risk for adverse health events.
Continued investment in AI and machine learning refines the company's ability to forecast health trends and personalize treatment pathways, vital for its integrated care model. Cybersecurity and data privacy are paramount, with robust defenses against breaches and strict HIPAA adherence crucial for maintaining patient trust and avoiding legal penalties.
Legal factors
Alignment Healthcare operates under stringent Centers for Medicare & Medicaid Services (CMS) regulations, particularly concerning its Medicare Advantage plans. These rules dictate everything from the benefits offered and how members enroll to marketing tactics and the accuracy of financial reporting.
Staying compliant with the annual CMS final rules is critical for continued operation. For instance, the 2025 contract year updates will introduce specific requirements that Alignment Healthcare must adhere to, impacting plan design and member outreach strategies.
Healthcare fraud and abuse laws, such as the False Claims Act, Anti-Kickback Statute, and Stark Law, are paramount for Alignment Healthcare. These regulations are designed to curb fraud, waste, and abuse within federal healthcare programs, necessitating rigorous compliance in all operational aspects, particularly physician and hospital relationships.
The U.S. Department of Justice (DOJ) and the Department of Health and Human Services (HHS) are actively pursuing healthcare fraud. In fiscal year 2023, the DOJ reported recovering over $1.8 billion in healthcare fraud settlements and judgments, underscoring the significant financial and legal risks associated with non-compliance for entities like Alignment Healthcare.
The Health Insurance Portability and Accountability Act (HIPAA) mandates strict protocols for safeguarding protected health information (PHI). Alignment Healthcare's commitment to robust data security and unwavering HIPAA compliance is critical for protecting member data, fostering trust, and preventing substantial financial penalties.
Violations of HIPAA can lead to severe consequences, including fines that can reach up to $1.5 million per violation category annually, as established by the HITECH Act. In 2023, the U.S. Department of Health and Human Services (HHS) reported settlements totaling over $40 million for HIPAA breaches, underscoring the financial risks associated with non-compliance.
Licensing and Accreditation Requirements
Alignment Healthcare, as a health plan operator, navigates a complex web of state-specific licensing mandates. For instance, in 2024, the company's operations across California, Arizona, Florida, and North Carolina necessitate adherence to each state's unique insurance department regulations for health insurers. Failure to maintain these licenses can halt operations in a given state.
Beyond state licensing, accreditations play a crucial role in establishing credibility and market access. Organizations like the National Committee for Quality Assurance (NCQA) offer accreditations for health plans, which are often a prerequisite for contracting with Medicare Advantage and Medicaid managed care programs. Alignment Healthcare's commitment to these accreditations, such as NCQA's Managed Care Organization accreditation, directly impacts its ability to serve government-sponsored beneficiaries, a significant portion of its member base.
- State-Specific Licensing: Alignment Healthcare must hold active health plan licenses in every state it operates, ensuring compliance with each state's insurance laws and regulations.
- Accreditation Importance: Industry accreditations, like those from NCQA, are vital for network participation and demonstrating a commitment to quality care, influencing member enrollment and provider contracts.
- Regulatory Compliance Costs: Maintaining compliance with diverse licensing and accreditation standards incurs significant administrative and operational costs, impacting profitability.
- Impact on Market Access: Successful navigation of these legal requirements directly determines Alignment Healthcare's ability to enter and expand within new state markets and participate in key government programs.
Consumer Protection and Patient Rights
Laws safeguarding consumer rights and patient access to care directly impact Alignment Healthcare's business. Regulations governing appeals, utilization management, and the delivery of extra benefits are particularly pertinent. For instance, in 2024, the Centers for Medicare & Medicaid Services (CMS) continued to emphasize robust member protections, with updated guidance on grievance and appeals processes potentially affecting how Alignment Healthcare handles member disputes.
Ensuring transparency and fair dealings with members is a legal requirement and crucial for maintaining member trust and satisfaction. This includes clear communication about plan benefits, out-of-pocket costs, and coverage decisions. Adherence to these standards is vital for avoiding regulatory penalties and fostering positive member relationships.
Key legal factors influencing Alignment Healthcare include:
- Consumer Protection Laws: Mandates for clear and accurate plan information, prohibiting deceptive marketing practices.
- Patient Rights Regulations: Rules dictating fair access to care, including timely approvals and transparent appeals processes.
- Utilization Management Standards: Legal frameworks that guide how healthcare services are reviewed and authorized, ensuring medical necessity.
- Supplemental Benefit Compliance: Regulations specifying the scope and delivery of additional benefits offered by Medicare Advantage plans, like transportation or dental coverage.
Alignment Healthcare operates within a highly regulated environment, subject to extensive federal and state laws. The Centers for Medicare & Medicaid Services (CMS) sets stringent rules for Medicare Advantage plans, impacting plan design, enrollment, and marketing. For example, the 2025 CMS final rule updates will necessitate adjustments to Alignment's strategies. Furthermore, laws like the False Claims Act and Anti-Kickback Statute are critical, with the DOJ recovering over $1.8 billion in healthcare fraud settlements in FY2023, highlighting the financial risks of non-compliance.
HIPAA compliance is paramount for protecting member data, with fines potentially reaching $1.5 million per violation category annually; HHS settlements for HIPAA breaches in 2023 exceeded $40 million. State-specific licensing, such as in California and Arizona in 2024, is essential for market access, and accreditations from bodies like NCQA are vital for contracting with government programs. Consumer protection laws, patient rights regulations, and utilization management standards also shape operations, with CMS emphasizing member protections and fair grievance processes.
| Legal Factor | Impact on Alignment Healthcare | Relevant Data/Example (2023-2025) |
| CMS Regulations (Medicare Advantage) | Dictates plan design, enrollment, marketing, and financial reporting. | 2025 CMS final rule updates will introduce new compliance requirements. |
| Healthcare Fraud & Abuse Laws (e.g., FCA, AKS) | Mandates rigorous compliance to avoid penalties. | DOJ recovered over $1.8 billion in healthcare fraud settlements in FY2023. |
| HIPAA Compliance | Requires robust data security for protected health information (PHI). | HHS settlements for HIPAA breaches exceeded $40 million in 2023; fines up to $1.5M/category/year. |
| State-Specific Licensing | Necessitates adherence to unique insurance regulations in each operating state. | Operations in California, Arizona, Florida, and North Carolina require specific state licenses in 2024. |
| Accreditations (e.g., NCQA) | Enhances credibility and is often required for government program participation. | NCQA accreditation impacts ability to serve Medicare Advantage beneficiaries. |
| Consumer Protection & Patient Rights | Ensures transparency, fair dealings, and access to care. | CMS guidance in 2024 emphasizes member protections in grievance and appeals processes. |
Environmental factors
Climate change presents indirect challenges for Alignment Healthcare by potentially increasing healthcare needs among its senior member base. Extreme weather events, such as heatwaves or severe storms, can lead to a rise in heat-related illnesses, respiratory problems exacerbated by poor air quality, and injuries, all of which would likely increase demand for healthcare services.
For instance, the Centers for Disease Control and Prevention (CDC) reported that in 2023, there were over 1,200 heat-related deaths in the United States, a significant portion of which likely affected vulnerable populations such as the elderly. This trend suggests a growing need for proactive health management and increased healthcare utilization that Alignment Healthcare must anticipate.
Alignment Healthcare faces growing pressure to integrate sustainability and Corporate Social Responsibility (CSR) into its operations. This focus impacts how customers, investors, and employees view the company. For instance, a 2024 survey indicated that 70% of consumers consider a company's environmental impact when making purchasing decisions, a trend likely to continue influencing healthcare providers.
While direct environmental impacts like emissions might not be Alignment Healthcare's core business, demonstrating environmental stewardship can significantly boost its brand image. For example, initiatives like reducing waste in administrative processes or promoting digital health solutions that lessen travel can be highlighted. Such efforts align with a broader societal expectation for businesses to contribute positively to the environment, potentially improving stakeholder perception and trust.
The COVID-19 pandemic underscored the profound impact of environmental health risks on seniors, a core demographic for Alignment Healthcare. The company's agility in adapting care delivery, such as broadening telehealth services, proved vital during these disruptive periods. For instance, in 2023, Alignment Healthcare reported a significant increase in telehealth utilization, demonstrating its capacity to maintain member access during health emergencies.
Looking ahead, the potential for future pandemics or widespread environmental health challenges presents a substantial risk to healthcare infrastructure. Such events could strain Alignment Healthcare's operational capacity and necessitate further innovation in care delivery to ensure continued support for its members, particularly the elderly.
Environmental Health Risks Affecting Seniors
Environmental factors like local air pollution and water quality can significantly impact the health of seniors, a demographic often more vulnerable to these risks. For instance, in 2024, the American Lung Association reported that over 130 million Americans live in areas with unhealthy air quality, a concern for older adults with pre-existing respiratory conditions.
Alignment Healthcare, while not directly controlling environmental conditions, can mitigate their effects on its senior members. This involves proactive care coordination and preventive health strategies that account for environmental exposures. Understanding that 20% of Medicare beneficiaries live in areas with poor air quality, as indicated by recent studies, highlights the importance of such measures.
- Air Quality: Seniors in areas with high levels of particulate matter (PM2.5) or ozone face increased risks of respiratory and cardiovascular issues.
- Water Contamination: Exposure to lead or other contaminants in drinking water can exacerbate age-related health problems.
- Extreme Heat: Rising global temperatures, with 2024 projected to be one of the hottest years on record, pose a significant heatstroke risk for seniors.
- Pesticides and Toxins: Proximity to agricultural areas or industrial sites can lead to exposure to harmful chemicals, impacting long-term health.
Resource Management in Healthcare Operations
The healthcare sector broadly impacts the environment through waste, energy use, and supply chains. For Alignment Healthcare, a Medicare Advantage provider, direct environmental impact stems from its administrative and care coordination functions. While not a primary operational concern, adopting sustainable resource management in these areas demonstrates corporate responsibility.
Even administrative operations contribute to environmental strain. Consider these areas:
- Waste Generation: Paper usage in claims processing, marketing materials, and general office supplies contributes to landfill waste. In 2024, the healthcare industry in the US generated an estimated 5.9 million tons of waste, with a significant portion being non-clinical.
- Energy Consumption: Data centers, office buildings, and remote work infrastructure all require electricity, leading to carbon emissions. The healthcare sector's energy consumption accounts for roughly 8.5% of total US greenhouse gas emissions.
- Supply Chain Footprint: While less direct for an MA plan, the procurement of office supplies, technology, and services involves upstream environmental impacts.
- Digital Footprint: Increased reliance on digital platforms and data storage has an energy cost associated with servers and network infrastructure.
Environmental factors like air quality and extreme weather pose direct health risks to Alignment Healthcare's senior members, increasing demand for services. For example, studies in 2024 indicated that over 130 million Americans live in areas with unhealthy air, a significant concern for older adults.
Alignment Healthcare's administrative operations, though not its core function, also have environmental impacts through waste generation and energy consumption. The healthcare industry's substantial waste, estimated at 5.9 million tons in the US in 2024, highlights the need for sustainable resource management.
The company's agility in adopting telehealth, as seen with increased utilization in 2023, demonstrates its capacity to adapt to environmental health challenges and ensure member access during disruptions, a critical factor given the potential for future pandemics.
Integrating sustainability and CSR is increasingly important, with 70% of consumers in a 2024 survey considering environmental impact in purchasing decisions, influencing stakeholder perception and trust.
PESTLE Analysis Data Sources
Our PESTLE Analysis for Alignment Healthcare is built on a robust foundation of data from government health agencies, regulatory bodies, and industry-specific market research reports. We incorporate insights from financial news outlets and economic forecasting firms to ensure a comprehensive understanding of the macro-environmental factors impacting the healthcare sector.