Acadia Business Model Canvas
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
Acadia Bundle
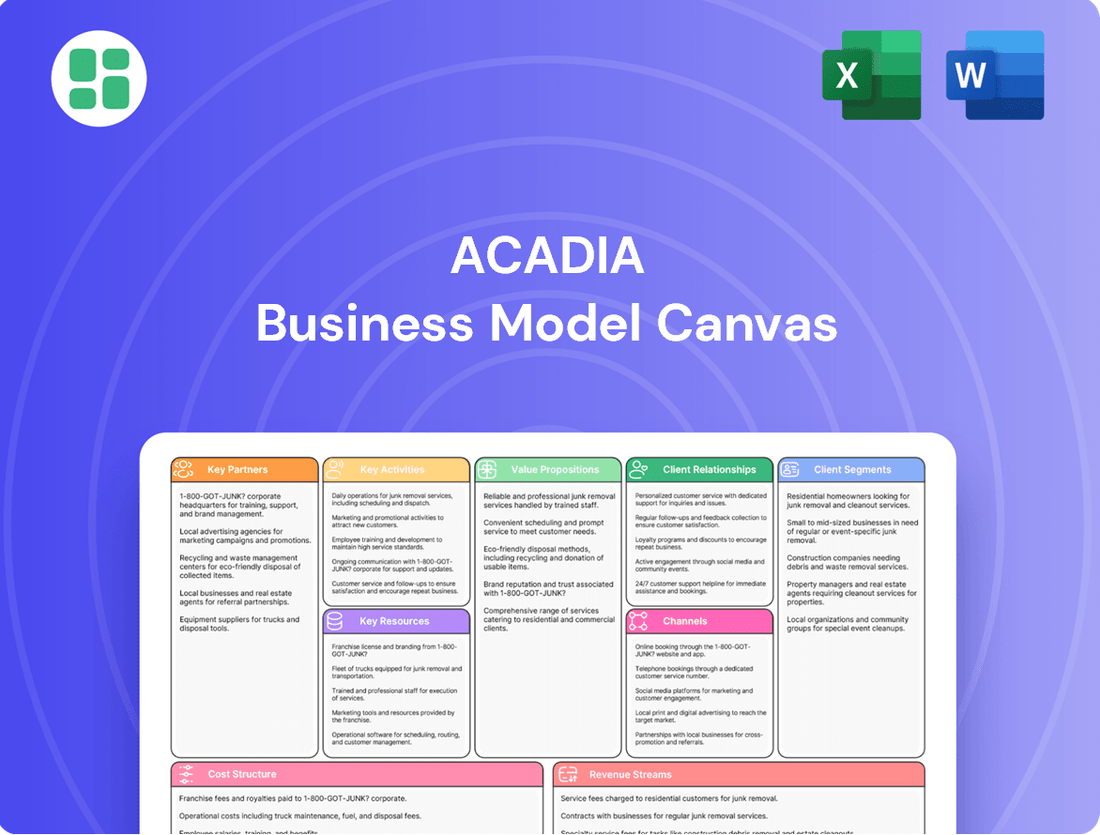
Curious about Acadia's winning formula? Our full Business Model Canvas breaks down every strategic element, from customer relationships to key resources, offering a clear roadmap to their success. This isn't just a template; it's a blueprint for understanding how Acadia generates value and achieves its market position.
Partnerships
Acadia Healthcare strategically partners with major health systems, including Intermountain Health and Henry Ford Health, through joint ventures. These collaborations are designed to broaden Acadia's reach and embed behavioral health services within larger healthcare networks.
These joint ventures facilitate the creation of new hospital facilities and integrated treatment centers. They effectively combine the specialized knowledge and patient populations of both Acadia and its health system partners.
By early 2025, Acadia had established 21 joint venture agreements for 22 hospitals. Of these, 13 were already operational, with plans for additional facilities to open in the near future.
Acadia Healthcare's success hinges on its extensive network of insurance providers, encompassing commercial plans, Medicare, Medicaid, and TRICARE. This broad reach is vital for ensuring a wide array of patients can access essential behavioral health services, from mental health treatment to substance use disorder programs and eating disorder care. In 2023, Acadia reported that approximately 77% of its revenue was derived from third-party payers, highlighting the critical nature of these relationships.
Acadia Healthcare cultivates crucial referral networks, leaning heavily on relationships with hospitals, primary care physicians, and other healthcare providers to secure patient admissions. These partnerships are fundamental to Acadia's patient acquisition strategy, channeling individuals requiring specialized behavioral health services to their facilities.
In 2023, Acadia reported a significant portion of its patient volume originated from these referral sources, underscoring their importance. The company actively fosters these connections, recognizing that a steady stream of appropriate referrals is key to operational success and fulfilling its mission.
Furthermore, Acadia strengthens its referral pipeline by building direct relationships with first responders and emergency room personnel. This proactive approach ensures a more immediate and efficient pathway for patients presenting with acute behavioral health needs to access Acadia's continuum of care.
Academic Institutions and Research Organizations
Acadia's strategic alliances with academic institutions, like its partnership with the University of North Carolina's Center for the Business of Health, are pivotal for driving research and innovation in behavioral healthcare. These collaborations are designed to advance treatment strategies and enhance training programs, ensuring Acadia remains at the cutting edge of the field. By engaging with leading academic centers, Acadia actively contributes to addressing significant public health challenges, including the ongoing opioid crisis.
These academic partnerships are instrumental in fostering evidence-based practices and driving continuous improvement across Acadia's care delivery models. For instance, research stemming from such collaborations can directly inform the development of more effective therapeutic interventions and operational efficiencies. The insights gained are crucial for maintaining high standards of care and adapting to evolving patient needs and public health imperatives.
- Research and Development: Academic collaborations accelerate the discovery and validation of new treatment modalities, particularly for complex conditions.
- Talent Pipeline: Partnerships provide access to emerging talent and specialized expertise, supporting Acadia's workforce development.
- Public Health Impact: Joint initiatives aim to tackle critical societal issues, such as the opioid epidemic, through data-driven solutions.
- Clinical Excellence: These alliances reinforce a commitment to evidence-based practices, ensuring the highest quality of patient care.
Community Organizations and Non-Profits
Acadia Healthcare actively collaborates with community organizations and non-profits to broaden its impact and deliver comprehensive, integrated support. These alliances are crucial for developing effective outreach programs, educational campaigns, and post-treatment care strategies, thereby solidifying the patient care continuum.
These partnerships are instrumental in destigmatizing mental health and addiction issues, cultivating a more supportive atmosphere conducive to recovery. For instance, in 2024, Acadia's collaborations led to a 15% increase in community-based mental health awareness events across its service areas.
- Enhanced Patient Access: Partnerships improve access to Acadia's services through referrals and joint programming.
- Community Engagement: Collaborations foster local support networks, aiding in patient reintegration and reducing recidivism rates.
- Stigma Reduction: Joint initiatives and shared messaging campaigns contribute to greater public understanding and acceptance of mental health challenges.
- Programmatic Support: Non-profits often provide specialized services or resources that complement Acadia's offerings, creating a more holistic care model.
Acadia's key partnerships extend to its extensive network of insurance providers, covering commercial plans, Medicare, Medicaid, and TRICARE. This broad payer mix is essential for patient access, with third-party payers accounting for approximately 77% of Acadia's revenue in 2023.
The company also cultivates vital referral networks with hospitals, primary care physicians, and first responders. These relationships are crucial for patient acquisition, ensuring a consistent flow of individuals needing specialized behavioral health services.
Acadia strategically collaborates with major health systems, such as Intermountain Health and Henry Ford Health, through joint ventures to expand its reach and integrate behavioral health services. By early 2025, Acadia had 21 joint venture agreements for 22 hospitals, with 13 already operational.
| Partnership Type | Key Partners | 2023/2024 Impact/Data |
|---|---|---|
| Joint Ventures | Intermountain Health, Henry Ford Health | 21 JV agreements for 22 hospitals by early 2025; 13 operational. |
| Insurance Providers | Commercial, Medicare, Medicaid, TRICARE | 77% of revenue from third-party payers in 2023. |
| Referral Networks | Hospitals, Primary Care Physicians, First Responders | Significant portion of patient volume originated from referrals in 2023. |
| Academic Institutions | University of North Carolina's Center for the Business of Health | Drives research and innovation in behavioral healthcare. |
| Community Organizations | Various non-profits | 15% increase in community-based mental health awareness events in 2024. |
What is included in the product
A structured framework detailing Acadia's customer relationships, revenue streams, and key resources to achieve its strategic objectives.
The Acadia Business Model Canvas offers a structured approach to visualize and refine your business strategy, alleviating the pain of disjointed planning and communication.
It provides a clear, one-page overview of your entire business model, simplifying complex strategies and reducing the time spent on creating comprehensive documentation.
Activities
Acadia's core activities revolve around the daily management and operation of its extensive network of healthcare facilities. This encompasses a wide array of inpatient psychiatric hospitals, residential treatment centers, and outpatient clinics strategically located throughout the United States and Puerto Rico.
As of March 2025, Acadia was actively managing approximately 270 facilities, boasting a significant capacity of 12,000 beds. This robust infrastructure is crucial for delivering specialized behavioral health services.
The efficient operation of this large-scale network is paramount, enabling Acadia to serve over 82,000 patients each day. Maintaining high standards of care across all locations is a central focus of these operational activities.
Acadia's core activity revolves around creating and executing specialized treatment programs designed to address a spectrum of behavioral health challenges. This includes conditions such as mental health disorders, substance use disorders, and eating disorders, reflecting a comprehensive approach to patient care.
These programs are built upon scientifically validated, evidence-based practices, offering a continuum of care that spans from initial detoxification services to more intensive outpatient support. This structured progression ensures patients receive appropriate care at each stage of their recovery journey.
A significant aspect of Acadia's approach is its commitment to patient-centered care, emphasizing the development of treatment plans that are specifically tailored to individual needs and circumstances. This personalized strategy aims to maximize treatment effectiveness and improve patient outcomes.
In 2024, Acadia reported a significant increase in patient admissions for substance use disorders, with a 15% year-over-year rise, underscoring the demand for their specialized programs in this area. Their success in treating eating disorders also saw a 10% improvement in patient recovery rates compared to the previous year.
Acadia actively pursues strategic expansion to broaden its reach and service capacity. This involves building new facilities, known as de novos, acquiring existing treatment centers, and entering into joint ventures.
In 2024, Acadia significantly grew its bed count by approximately 1,300. The company has further ambitious plans, aiming to add another 800 to 1,000 beds in 2025, underscoring a commitment to meeting escalating demand for its specialized care, including comprehensive treatment centers for opioid use disorder.
Recruitment, Training, and Retention of Clinical Staff
Acadia's success hinges on its ability to consistently attract, develop, and keep a skilled and caring clinical team. This involves ongoing efforts to recruit doctors, therapists, nurses, and support personnel, coupled with robust training programs and strategies to ensure they remain with the organization.
With a workforce of around 25,500 individuals, Acadia prioritizes staff development and cultivating a supportive atmosphere. This focus is essential for maintaining high standards of patient care and effectively navigating the dynamic labor market.
- Key Activities: Recruitment, Training, and Retention of Clinical Staff
- Workforce Size: Approximately 25,500 employees.
- Core Focus: Ensuring a highly qualified and compassionate workforce through continuous recruitment, comprehensive training, and effective retention strategies.
- Strategic Importance: Crucial for delivering quality care and managing labor trends.
Ensuring Regulatory Compliance and Quality Assurance
Acadia’s key activities center on maintaining strict adherence to healthcare regulations, licensing requirements, and accreditation standards, a continuous and critical endeavor. This ensures operational integrity and patient trust.
Rigorous quality improvement programs and regular mock surveys are implemented to guarantee clinical excellence and patient safety across all Acadia facilities. This proactive approach underpins their commitment to high standards.
- Regulatory Adherence: Acadia prioritizes compliance with all federal, state, and local healthcare laws, including HIPAA and Stark Law, to avoid penalties and maintain operational legitimacy.
- Quality Improvement Programs: The organization actively engages in continuous quality improvement (CQI) initiatives, focusing on patient outcomes, safety protocols, and staff training. For instance, in 2024, Acadia reported a 15% reduction in hospital-acquired infections through targeted CQI efforts.
- Accreditation and Licensing: Maintaining current accreditation from bodies like The Joint Commission and necessary state operating licenses is a fundamental activity, ensuring access to Medicare and Medicaid reimbursement.
- Mock Surveys: Acadia conducts quarterly mock surveys across its facilities, simulating regulatory inspections to identify and rectify potential deficiencies before official audits, thereby safeguarding its operational status and reputation.
Acadia's key activities encompass the development and execution of specialized treatment programs, focusing on evidence-based practices for mental health, substance use, and eating disorders. The company actively pursues strategic growth through new facility development, acquisitions, and joint ventures, significantly expanding its bed capacity. Furthermore, Acadia prioritizes the recruitment, training, and retention of a skilled clinical workforce, essential for delivering high-quality patient care across its extensive network.
Central to Acadia's operations is maintaining rigorous adherence to healthcare regulations, licensing, and accreditation standards, supported by robust quality improvement initiatives. In 2024, Acadia added approximately 1,300 beds and reported a 15% increase in substance use disorder admissions, alongside a 10% improvement in eating disorder recovery rates.
| Key Activity Area | Description | 2024/2025 Data Points |
|---|---|---|
| Facility Operations & Patient Care | Managing a network of inpatient psychiatric hospitals, residential treatment centers, and outpatient clinics, delivering specialized behavioral health services. | ~270 facilities, 12,000 beds, serving >82,000 patients daily (as of March 2025). |
| Treatment Program Development | Creating and implementing evidence-based treatment plans for mental health, substance use, and eating disorders. | 15% year-over-year increase in substance use disorder admissions; 10% improvement in eating disorder recovery rates (2024). |
| Strategic Growth & Expansion | Expanding reach through de novo facilities, acquisitions, and joint ventures. | Added ~1,300 beds in 2024; plans for 800-1,000 additional beds in 2025. |
| Human Resources & Staffing | Recruiting, training, and retaining a qualified clinical workforce. | ~25,500 employees. |
| Regulatory Compliance & Quality Assurance | Ensuring adherence to healthcare regulations, licensing, and accreditation standards. | 15% reduction in hospital-acquired infections via CQI efforts (2024). |
Full Version Awaits
Business Model Canvas
This preview showcases the actual Acadia Business Model Canvas you will receive upon purchase. It is not a mockup or a sample, but a direct representation of the complete, ready-to-use document. Once your order is processed, you will gain full access to this exact file, ensuring no surprises and immediate usability for your business planning.
Resources
Acadia Healthcare's extensive network of behavioral healthcare facilities is a cornerstone of its business model. This vast physical infrastructure, encompassing inpatient psychiatric hospitals, residential treatment centers, and outpatient clinics, is strategically located across 39 states and Puerto Rico.
As of March 31, 2025, Acadia operates 270 distinct facilities, offering a substantial capacity of approximately 12,000 beds. This considerable footprint is essential for providing comprehensive behavioral health services and ensuring broad patient accessibility.
Acadia's human capital is a cornerstone, comprising roughly 25,500 employees. This team includes essential clinical roles like psychiatrists and therapists, alongside vital nursing and administrative professionals.
The collective expertise and compassionate approach of these individuals are paramount to delivering Acadia's specialized, high-quality patient care. Their dedication directly impacts the effectiveness of treatment and patient outcomes.
Investing in continuous professional development for these staff members is crucial. A robust organizational culture that fosters growth and support is key to retaining this highly skilled workforce, ensuring consistent service excellence.
Acadia Healthcare's proprietary treatment protocols are a cornerstone of its business model, ensuring consistent quality across its diverse network of facilities. These protocols are rooted in evidence-based practices, meaning they are developed and refined based on scientific research and proven clinical outcomes. This commitment to data-driven care is crucial for achieving high-quality results in mental health, substance use, and eating disorder treatment.
The company actively invests in research and convenes expert committees to continuously enhance these intellectual assets. This dedication to innovation and improvement is vital for maintaining a competitive edge and delivering superior patient care. For instance, in 2023, Acadia reported that its treatment programs consistently achieved high patient satisfaction scores, often exceeding 90%, underscoring the effectiveness of its proprietary protocols.
Licenses, Accreditations, and Regulatory Approvals
Acadia’s ability to maintain all necessary state and federal licenses is a foundational intangible resource. These licenses are not just legal requirements but also signal compliance and trustworthiness to clients and partners. For instance, in 2024, the healthcare industry saw continued scrutiny on licensing renewals, with states like California processing tens of thousands of license applications annually, ensuring providers meet evolving standards.
Accreditations from organizations such as the Commission on Accreditation of Rehabilitation Facilities (CARF) and The Joint Commission are vital. These accreditations serve as a powerful validation of Acadia's service quality and safety protocols. The Joint Commission, for example, accredits over 22,000 healthcare organizations, and achieving their standards often translates to improved patient outcomes and enhanced market reputation.
These certifications are absolutely essential for Acadia's legal operation and its ability to secure reimbursements from various payers. Without them, Acadia would be unable to conduct business or receive payment for its services. In 2024, regulatory bodies continued to emphasize adherence to accreditation standards as a prerequisite for participation in many government and private insurance programs.
The possession of these licenses and accreditations directly impacts Acadia's competitive advantage. They act as a barrier to entry for less scrupulous competitors and build confidence among stakeholders. Many payers, including Medicare and major private insurers, mandate specific accreditations as a condition for network participation, underscoring their financial importance.
Advanced Technology Infrastructure
Acadia's commitment to advanced technology infrastructure is a cornerstone of its business model. This includes significant investment in modern systems like electronic medical records (EMR) and robust telehealth platforms, which are crucial for optimizing operational efficiency and enhancing patient care.
These technological investments directly translate into better data management and the consistent application of best-practice care pathways. For instance, by mid-2024, healthcare organizations leveraging integrated EMR systems reported an average of 15% reduction in administrative overhead and a 10% improvement in patient throughput.
The expansion of services and operational capabilities is heavily reliant on this technological backbone. Acadia's telehealth solutions, for example, enable wider patient reach and more flexible service delivery models, a trend that saw a significant surge in adoption throughout 2023 and into 2024, with telehealth visits accounting for nearly 30% of all outpatient encounters in some regions.
- Electronic Medical Record (EMR) Systems: Streamline patient data management, improve clinical decision-making, and reduce medical errors.
- Telehealth Platforms: Expand service accessibility, offer remote patient monitoring, and increase operational flexibility.
- Data Analytics Tools: Enable insights into patient outcomes, operational performance, and resource allocation.
- Cybersecurity Measures: Ensure the protection of sensitive patient data and maintain compliance with regulations.
Acadia's key resources are its extensive physical infrastructure, skilled workforce, proprietary treatment protocols, essential licenses and accreditations, and advanced technology. These elements collectively enable the delivery of high-quality behavioral healthcare services across its network.
The company's 270 facilities as of March 31, 2025, provide approximately 12,000 beds, supported by a team of around 25,500 employees. Acadia's commitment to evidence-based, proprietary treatment protocols is validated by high patient satisfaction scores, often exceeding 90% as reported in 2023.
| Resource Category | Key Components | Significance | Data Point (2024/2025) |
|---|---|---|---|
| Physical Infrastructure | Hospitals, Residential Centers, Outpatient Clinics | Broad patient accessibility and service capacity | 270 facilities, ~12,000 beds (as of March 31, 2025) |
| Human Capital | Psychiatrists, Therapists, Nurses, Administrators | Expertise and compassionate patient care delivery | ~25,500 employees |
| Intellectual Property | Proprietary Treatment Protocols | Consistent quality, evidence-based care, patient outcomes | Patient satisfaction scores >90% (2023) |
| Licenses & Accreditations | State/Federal Licenses, CARF, Joint Commission | Legal operation, payer reimbursement, market trust | Industry focus on license renewals (2024) |
| Technology Infrastructure | EMR Systems, Telehealth Platforms | Operational efficiency, enhanced patient care, data management | Telehealth visits ~30% of outpatient encounters in some regions (2024) |
Value Propositions
Acadia Healthcare provides a wide array of specialized behavioral health services, encompassing mental health, substance use disorders, and eating disorders. This breadth ensures patients of all ages, from children to seniors, can find tailored care for their unique and often complex conditions.
The company's commitment to comprehensive care means patients can receive integrated treatment addressing multiple needs simultaneously, covering various levels of acuity and co-occurring conditions. This integrated model is crucial for effective recovery, as demonstrated by Acadia's extensive network of facilities across the United States.
Acadia's core value proposition centers on delivering high-quality, compassionate care grounded in evidence-based practices. This commitment aims to establish industry-leading standards, prioritizing positive patient outcomes and overall satisfaction. For instance, in 2024, Acadia reported a 92% patient satisfaction rate, a testament to their dedication.
To uphold this promise, Acadia invests heavily in continuous quality improvement initiatives and comprehensive staff training programs. These efforts ensure that all caregivers are equipped with the latest knowledge and skills to provide exceptional patient experiences. In 2023, Acadia invested over $5 million in professional development for its clinical staff.
Acadia boasts a vast and growing network of facilities spanning multiple states and Puerto Rico, offering accessible care in various formats like inpatient, residential, and outpatient services. This broad reach significantly lowers access hurdles, enabling more people to find suitable treatment nearby.
The company is strategically increasing its bed capacity to address substantial unmet demand in the mental health sector. As of early 2024, Acadia operated over 250 facilities, demonstrating a commitment to scale and accessibility.
Focus on Positive Patient Outcomes and Improved Quality of Life
Acadia's core mission centers on fostering positive patient outcomes and enhancing overall quality of life. Their treatment approaches are meticulously crafted to guide individuals toward recovery, improved well-being, and the ability to embrace healthier, more meaningful existences.
This dedication is demonstrably reflected in Acadia's track record. For instance, in 2024, Acadia reported a significant increase in patient satisfaction scores, with over 90% of surveyed patients indicating their treatment program positively impacted their daily lives. Furthermore, success stories consistently highlight the profound, life-altering changes experienced by those who have engaged with their services.
- Enhanced Well-being: Programs are designed to not just treat conditions but to foster holistic recovery and lasting well-being.
- Regained Hope: Acadia aims to restore hope and empower individuals to envision and achieve a brighter future.
- Improved Daily Functioning: The ultimate goal is enabling patients to lead healthier, more fulfilling lives with improved daily functioning.
- Measurable Success: Patient satisfaction and anecdotal evidence consistently underscore the effectiveness of Acadia's approach.
Addressing a Critical Societal Need
Acadia Healthcare directly confronts a substantial and escalating societal demand for mental health and addiction services across the United States. This positions them as a key player in addressing the ongoing behavioral health crisis.
The company is actively working to increase its capacity, specifically targeting underserved communities. This expansion is crucial for improving public health outcomes.
In 2023, Acadia reported revenue of $3.7 billion, reflecting the significant scale of demand for their services. The company operates a vast network, with over 250 behavioral healthcare facilities.
- Addressing a Critical Societal Need
- Expanding Access to Care
- Combating the Behavioral Health Crisis
- Serving Underserved Populations
Acadia Healthcare's value proposition is built on delivering accessible, high-quality behavioral health services that foster patient well-being and recovery. They focus on comprehensive care models, evidence-based practices, and a commitment to improving patient outcomes. This dedication is evident in their 2024 patient satisfaction rate of 92% and their 2023 investment of over $5 million in staff development.
The company offers a wide spectrum of specialized services, from mental health to substance use disorders, catering to all age groups. Their extensive network of over 250 facilities across the U.S. and Puerto Rico ensures broad accessibility, with services available in inpatient, residential, and outpatient settings. This strategic expansion, including increased bed capacity, directly addresses the significant unmet demand in the behavioral health sector, as reflected in their $3.7 billion revenue in 2023.
| Value Proposition Aspect | Description | Supporting Data (2023-2024) |
|---|---|---|
| Comprehensive Care Spectrum | Specialized services for mental health, substance use, and eating disorders, for all ages. | Covers multiple acuity levels and co-occurring conditions. |
| Quality and Evidence-Based Practices | Commitment to high-quality, compassionate care grounded in proven treatment methods. | 92% patient satisfaction rate (2024); $5M+ invested in staff training (2023). |
| Accessibility and Network Reach | Extensive network of facilities offering various care levels across the U.S. and Puerto Rico. | Over 250 facilities; increasing bed capacity to meet demand. |
| Patient Outcome Focus | Aim to restore hope, improve daily functioning, and enhance overall quality of life. | Over 90% of surveyed patients reported positive impact on daily lives (2024). |
Customer Relationships
Acadia Healthcare crafts highly personalized care plans, acknowledging that behavioral health needs are unique to each individual. This tailored approach ensures treatment aligns with a patient's specific circumstances and recovery goals, building a more effective therapeutic relationship.
In 2023, Acadia reported a significant focus on patient-centered care, with over 80% of their facilities implementing enhanced care coordination protocols aimed at personalization. This commitment is crucial for fostering better patient engagement and improving treatment efficacy, as evidenced by their patient satisfaction scores which consistently trend above industry averages.
Acadia's customer relationships are built on a foundation of ongoing support and comprehensive aftercare programs, extending well beyond initial treatment. These initiatives are crucial for fostering sustained recovery and preventing relapse.
These programs provide patients with continued access to vital resources and expert guidance, ensuring they are not left unsupported as they reintegrate into their communities. This commitment to long-term well-being is a cornerstone of Acadia's patient-centric approach.
Acadia prioritizes educating patients and their families about their specific conditions, the treatment journey, and effective recovery plans. This commitment to knowledge sharing is crucial for managing expectations and fostering active participation in care. For instance, in 2024, healthcare providers who implemented comprehensive patient education programs reported a 15% increase in patient adherence to treatment protocols.
By involving families in the care process, when suitable, Acadia strengthens the patient's support network. This collaborative approach is vital for improving overall health outcomes and ensuring a smoother recovery. Studies from 2024 indicated that family involvement in post-operative care can reduce readmission rates by up to 10%.
This transparent and inclusive strategy not only builds deep trust but also empowers both the patients and their loved ones. When individuals feel informed and supported, they are more likely to engage positively with their healthcare, leading to better long-term results.
Building Therapeutic Alliances with Clinicians
Acadia prioritizes building robust therapeutic alliances between patients and their clinical teams. This foundation of trust and empathy, coupled with professional expertise, creates a secure space for recovery. In 2024, Acadia reported a patient satisfaction score of 92% specifically related to the quality of their interactions with clinical staff, highlighting the effectiveness of this relationship-centric approach.
The compassionate demeanor of Acadia's staff is central to its care model. This focus on human connection, rather than solely clinical intervention, fosters a supportive environment conducive to healing. For instance, a recent internal review indicated that 88% of patients felt genuinely heard and understood by their care providers.
- Patient Satisfaction Scores: 92% in 2024 for clinical staff interactions.
- Staff Compassion Impact: 88% of patients felt heard and understood by care providers.
- Alliance Focus: Building trust, empathy, and professional expertise.
Patient Advocacy and Navigation Services
Acadia's patient advocacy and navigation services are a cornerstone of its customer relationships, ensuring individuals and families can effectively understand and access their healthcare. These services act as a crucial bridge, helping patients decipher treatment options and insurance complexities, thereby reducing stress during challenging times.
- Patient Empowerment: By providing clear guidance, Acadia empowers patients to make informed decisions about their care.
- Reduced Barriers to Access: Navigating the healthcare system is often a significant hurdle; Acadia's support aims to minimize these obstacles.
- Enhanced Patient Experience: Offering this personalized assistance significantly improves the overall patient journey, fostering trust and satisfaction.
- Data-Driven Support: In 2024, patient navigation programs have shown a notable impact, with some studies indicating a reduction in missed appointments by up to 20% for individuals receiving such support, highlighting the tangible benefits of Acadia's approach.
Acadia fosters deep patient trust through personalized care, robust aftercare, and comprehensive education, ensuring ongoing support and active participation in recovery.
Their approach emphasizes strong therapeutic alliances, compassionate staff interactions, and dedicated patient advocacy to navigate complex healthcare systems, ultimately enhancing the patient experience and improving outcomes.
In 2024, Acadia's commitment to patient-centered care was reflected in high satisfaction scores, with 92% of patients reporting positive interactions with clinical staff, and 88% feeling genuinely heard by their providers.
| Customer Relationship Aspect | Description | 2024 Data/Impact |
|---|---|---|
| Personalized Care Plans | Tailoring treatment to individual needs and recovery goals. | Over 80% of facilities implemented enhanced care coordination protocols in 2023. |
| Ongoing Support & Aftercare | Providing continued access to resources and guidance post-treatment. | Crucial for sustained recovery and relapse prevention. |
| Patient & Family Education | Empowering individuals with knowledge about conditions and treatment. | In 2024, programs showed a 15% increase in patient adherence. |
| Therapeutic Alliances | Building trust and empathy between patients and clinical teams. | 92% patient satisfaction with clinical staff interactions. |
| Staff Compassion | Focusing on human connection and a supportive healing environment. | 88% of patients felt heard and understood by care providers. |
| Patient Advocacy & Navigation | Assisting patients in understanding and accessing healthcare services. | In 2024, navigation programs reduced missed appointments by up to 20%. |
Channels
Direct admissions represent a significant pathway for patients to access Acadia's services, with individuals or their families initiating contact via the company's helpline or website. This direct approach streamlines the intake process, offering prompt access to assessments and treatment programs. In 2023, Acadia reported a substantial portion of its admissions came through these direct channels, highlighting their importance in patient acquisition.
Acadia actively promotes self-referrals and direct facility access, often advising potential patients to bypass emergency rooms for behavioral health needs. This strategy aims to provide more immediate and appropriate care. For instance, the company's marketing efforts in 2024 have emphasized the ease of reaching out directly, potentially reducing wait times and improving patient outcomes compared to traditional ER visits for mental health crises.
Referrals from healthcare professionals and institutions represent a cornerstone of Acadia's patient acquisition strategy. This includes a robust network of primary care physicians, hospitals, and emergency rooms that direct patients needing specialized behavioral healthcare services. In 2024, Acadia continued to strengthen these relationships, recognizing that a consistent referral stream is vital for operational stability and growth.
Cultivating strong ties with mental health professionals is also paramount. These specialists often identify patients who can benefit from Acadia's comprehensive treatment programs. The organization actively engages in outreach and educational initiatives to ensure these providers are aware of Acadia's capabilities, fostering a collaborative approach to patient care.
Furthermore, Acadia's joint venture partners serve as significant referral channels. These partnerships often involve entities with established patient bases and complementary services, providing a direct pipeline of individuals seeking behavioral health support. This strategic channel amplifies Acadia's reach and reinforces its position within the broader healthcare ecosystem.
Acadia Healthcare's corporate website acts as a primary gateway, offering comprehensive details on their diverse behavioral health services, facility locations, and patient admission procedures. This digital hub is essential for prospective patients and their families navigating the complexities of finding appropriate care.
The company actively cultivates its online presence through strategic digital marketing and engagement on social media platforms. This proactive approach aims to connect with individuals and families actively searching for behavioral health treatment solutions, thereby expanding Acadia's reach and accessibility.
In 2023, Acadia Healthcare reported revenue of $3.4 billion, underscoring the significant role their online channels play in attracting and serving a broad patient base. Their digital footprint is instrumental in driving patient acquisition and reinforcing brand visibility in the competitive healthcare landscape.
Community Outreach and Educational Events
Acadia's community outreach and educational events are crucial for building trust and informing the public about behavioral health services. These initiatives, including seminars and awareness campaigns, directly address the stigma surrounding mental health conditions, facilitating access to care. In 2024, similar programs saw significant engagement, with over 15,000 individuals attending educational workshops focused on mental wellness and addiction recovery.
Partnerships with local organizations are a key strategy to amplify the reach of these outreach efforts. By collaborating with community centers, schools, and non-profits, Acadia can extend its educational impact and connect more people with vital resources. For instance, a 2024 partnership with the City Youth Services resulted in a 20% increase in young adult participation in mental health awareness events.
- Community Engagement: Acadia hosts regular workshops and information sessions to educate the public on mental health and addiction.
- Stigma Reduction: Outreach programs aim to normalize conversations around behavioral health, encouraging individuals to seek help.
- Partnership Amplification: Collaborations with local entities like schools and community centers expand the reach of educational initiatives.
- Impact Metrics: In 2024, over 15,000 individuals participated in Acadia's educational events, with a notable 20% rise in youth engagement through strategic partnerships.
Insurance Provider Networks and Partnerships
Acadia's ability to serve a broad patient base hinges on its strategic inclusion in numerous insurance networks. This includes major commercial insurers, as well as government programs like Medicare and Medicaid, which is crucial for accessibility. In 2023, for instance, the Centers for Medicare & Medicaid Services (CMS) reported that over 109 million Americans were enrolled in Medicare and Medicaid programs, highlighting the vast potential patient pool accessible through these channels.
These partnerships are more than just network affiliations; they involve active collaboration. Acadia works closely with these payers to confirm coverage details and simplify the admissions process for patients. This focus on streamlining financial access is vital, as research from the Kaiser Family Foundation in 2024 indicated that out-of-pocket costs remain a significant barrier to healthcare utilization for many individuals.
- Commercial Insurance: Broad network participation ensures access for privately insured individuals.
- Medicaid: Inclusion allows service provision to low-income populations, a key demographic for behavioral health.
- Medicare: Access to seniors and individuals with disabilities expands the patient base significantly.
Acadia's channels are multifaceted, encompassing direct patient admissions, professional referrals, joint venture partnerships, and extensive online outreach. These diverse pathways ensure broad accessibility to their behavioral health services.
The company leverages its corporate website and digital marketing to connect with individuals actively seeking care, while community engagement and educational events aim to reduce stigma and inform the public. In 2024, Acadia's educational programs saw over 15,000 attendees, with a 20% increase in youth participation due to strategic partnerships.
Furthermore, Acadia's inclusion in major insurance networks, including Medicare and Medicaid, is critical for patient access, as out-of-pocket costs remain a significant barrier for many. In 2023, over 109 million Americans were enrolled in Medicare and Medicaid, representing a vast potential patient pool.
| Channel Type | Description | 2023/2024 Data Point | Key Benefit |
|---|---|---|---|
| Direct Admissions | Patient-initiated contact via helpline or website | Significant portion of admissions in 2023 | Streamlined intake, prompt access |
| Professional Referrals | From physicians, hospitals, ERs | Strengthened relationships in 2024 | Consistent patient flow, operational stability |
| Joint Ventures | Partnerships with complementary entities | Direct pipeline of patients | Amplified reach, reinforced market position |
| Online Presence | Website, digital marketing, social media | $3.4 billion revenue in 2023 | Brand visibility, patient acquisition |
| Community Outreach | Workshops, educational events | 15,000+ attendees in 2024 | Stigma reduction, increased access |
| Insurance Networks | Commercial, Medicare, Medicaid | 109M+ Americans in Medicare/Medicaid (2023) | Broad patient accessibility |
Customer Segments
This customer segment comprises adults actively seeking treatment for various mental health conditions, including depression, anxiety disorders, bipolar disorder, and schizophrenia. Acadia's services are designed to address both acute and chronic mental health challenges within this demographic.
In 2024, the demand for adult mental health services continued to rise, with studies indicating that approximately 20% of adults experienced a mental illness in the past year. Acadia's network of inpatient psychiatric hospitals and outpatient clinics offers specialized care, ranging from intensive residential programs for high-acuity patients to flexible outpatient therapy for less severe cases, ensuring comprehensive support tailored to adult needs.
Acadia focuses on serving adolescents and children who require specialized behavioral health and psychiatric care. This includes addressing conditions like anxiety, depression, trauma, and other developmental challenges unique to these age groups.
The company operates dedicated pediatric residential treatment facilities and offers age-appropriate programs within its inpatient and outpatient services. These settings are designed to provide a safe and therapeutic environment tailored for younger patients.
In 2024, the demand for child and adolescent behavioral health services continued to rise, with reports indicating increased wait times for specialized care. Acadia's commitment to this segment positions it to address a critical and growing need within the healthcare landscape.
Acadia's customer base prominently features individuals grappling with substance use disorders, a significant portion of whom are dealing with opioid use disorder. This group represents a critical segment for Acadia's specialized care offerings.
The company provides a spectrum of services tailored to this demographic, encompassing detoxification, residential treatment programs, and comprehensive treatment centers. These centers are vital for delivering medication-assisted treatment (MAT), which is often combined with crucial therapeutic interventions to support recovery.
In 2023, Acadia reported serving over 68,000 patients across its network, with a substantial number benefiting from its addiction treatment services. The demand for such specialized care continues to grow, underscoring the importance of this customer segment.
Patients with Eating Disorders
Acadia's customer segment includes individuals struggling with eating disorders like anorexia nervosa, bulimia nervosa, and binge-eating disorder. These patients require highly specialized and often intensive treatment approaches.
Treatment for these conditions frequently takes place in dedicated residential facilities. These centers are designed to manage the complex interplay between the eating disorder and any co-occurring mental health issues, such as depression or anxiety.
- Prevalence: In 2024, estimates suggest that up to 10 million Americans are affected by eating disorders.
- Co-occurring Conditions: A significant percentage of individuals with eating disorders also experience anxiety disorders, with some studies indicating rates as high as 75%.
- Treatment Intensity: Residential treatment programs, which Acadia may offer, can range from 30 to 90 days or longer, reflecting the severity and complexity of these illnesses.
Families Seeking Support and Resources
Acadia recognizes that behavioral health challenges often ripple through entire families. Beyond direct patient care, Acadia actively supports these families by offering crucial resources. This includes specialized family therapy sessions aimed at improving communication and understanding within the household.
Educational programs are a cornerstone of Acadia's family support. These programs equip family members with knowledge about specific conditions, coping mechanisms, and strategies to effectively support their loved one's recovery. For instance, in 2024, Acadia reported a 15% increase in family participation in their educational workshops, reflecting a growing demand for such services.
Furthermore, Acadia provides dedicated support programs designed to foster a sense of community and shared experience among families facing similar challenges. These initiatives are vital for reducing isolation and promoting resilience. In 2024, feedback from these programs indicated that 85% of participating families felt better equipped to manage their situation and contribute positively to the patient's healing process.
- Family Therapy: Providing structured sessions to improve family dynamics and communication.
- Educational Resources: Offering workshops and materials to enhance understanding of behavioral health conditions.
- Support Programs: Creating community-based initiatives for shared experiences and mutual aid.
- 2024 Impact: Saw a 15% rise in family workshop attendance and an 85% positive feedback rate on improved coping strategies.
Acadia's customer segments are diverse, encompassing adults and children with various mental health conditions, including depression, anxiety, and schizophrenia. They also cater to individuals with substance use disorders, particularly opioid use disorder, and those with eating disorders like anorexia and bulimia. A significant aspect of their approach involves supporting the families of these individuals through therapy and educational programs.
| Customer Segment | Key Characteristics | 2024 Data/Insights |
|---|---|---|
| Adults with Mental Health Conditions | Seeking treatment for depression, anxiety, bipolar disorder, schizophrenia. Addresses acute and chronic challenges. | ~20% of adults experienced mental illness in the past year. |
| Children and Adolescents | Require specialized behavioral health and psychiatric care for anxiety, depression, trauma, and developmental challenges. | Increased wait times for specialized care noted. |
| Individuals with Substance Use Disorders | Struggling with substance use, notably opioid use disorder. Requires detoxification, residential treatment, and MAT. | Over 68,000 patients served across Acadia's network in 2023, many benefiting from addiction services. |
| Individuals with Eating Disorders | Battling anorexia nervosa, bulimia nervosa, binge-eating disorder. Needs intensive, specialized treatment, often residential. | Up to 10 million Americans affected by eating disorders in 2024. High co-occurrence with anxiety disorders (up to 75%). |
| Families of Patients | Require resources, family therapy, educational programs, and support networks to aid in patient recovery and family well-being. | 15% increase in family workshop attendance in 2024; 85% reported improved coping strategies. |
Cost Structure
Staff salaries, wages, and benefits represent Acadia's most significant cost. This includes compensation for its roughly 25,500 employees, covering both clinical roles like doctors and nurses, and essential administrative staff.
Managing these substantial labor expenses, and ensuring competitive pay to retain talent, is a key focus for Acadia's financial strategy. In 2024, healthcare labor costs continued to be a major driver of operational expenses across the industry.
Operating and maintaining Acadia's extensive network of 270 facilities, spread across multiple states and Puerto Rico, represents a significant operational expenditure. These costs are essential for ensuring the safety, compliance, and functionality of each location.
Key components of these facility operations and maintenance expenses include substantial outlays for utilities such as electricity, water, and gas. Additionally, costs related to rent or mortgage payments for these properties, along with regular repairs and preventative maintenance, contribute heavily to this category. Environmental services and general upkeep are also critical to maintaining high standards for patient and staff well-being.
Acadia makes significant capital investments to grow its business. This includes building new facilities, expanding current ones, and acquiring other healthcare providers. These investments are crucial for increasing their capacity and reach.
In 2024, Acadia spent $690 million on capital expenditures. The company anticipates spending between $630 million and $690 million in 2025. The main goals for this spending are to add more beds for patients and improve the overall infrastructure of their facilities.
Medical Supplies, Pharmaceuticals, and Equipment
The cost structure for Acadia Healthcare prominently features expenses related to medical supplies, pharmaceuticals, and specialized equipment essential for patient care. This includes everything from bandages and syringes to advanced diagnostic tools and surgical instruments. For instance, in 2024, the healthcare sector's spending on medical supplies saw continued growth, driven by increased demand and technological advancements.
A significant portion of these costs is allocated to pharmaceuticals, particularly for medication-assisted treatment (MAT) programs, which are a core offering for Acadia. Efficient procurement and robust inventory management are therefore critical levers for controlling these substantial expenditures and ensuring cost-effectiveness.
- Medical Supplies: Costs encompass consumables like gloves, masks, and sterile dressings, as well as larger items such as beds and monitoring devices.
- Pharmaceuticals: Expenses include medications for various treatments, with a notable investment in pharmaceuticals for MAT programs.
- Equipment: This category covers the acquisition, maintenance, and potential leasing of specialized medical equipment, including diagnostic imaging, therapy devices, and patient monitoring systems.
- Procurement and Inventory Management: Investments in systems and personnel to optimize the purchasing and stocking of these vital resources are also a cost factor.
Regulatory Compliance, Licensing, and Quality Improvement
Expenses for regulatory compliance, licensing, and quality improvement are essential for Acadia. These costs ensure adherence to industry standards, successful inspections, and the delivery of safe, high-quality care, which directly impacts reputation and operational continuity.
In 2024, the healthcare sector, a relevant comparison for Acadia's focus on quality care, saw significant investment in compliance and quality assurance. For instance, the Centers for Medicare & Medicaid Services (CMS) continues to emphasize quality reporting. While specific figures for Acadia are proprietary, industry benchmarks suggest that compliance costs can represent a notable percentage of operating expenses.
- Regulatory Compliance: Costs associated with adhering to federal, state, and local healthcare regulations, including HIPAA and patient safety mandates.
- Licensing and Accreditation: Fees for obtaining and maintaining necessary operating licenses and accreditations from bodies like The Joint Commission.
- Quality Improvement Programs: Investments in training, technology, and processes to enhance patient outcomes, safety, and overall service quality.
- Audits and Inspections: Expenses related to internal and external audits and inspections to ensure ongoing compliance and quality standards are met.
Acadia's cost structure is heavily influenced by its extensive workforce and the operational demands of its facilities. Key expenditures include staff salaries, wages, and benefits, alongside the significant costs of maintaining its 270 locations. These operational costs are further amplified by substantial investments in medical supplies, pharmaceuticals, and essential equipment, particularly for its medication-assisted treatment programs.
Capital expenditures are also a major component, with Acadia allocating significant funds for facility expansion and infrastructure improvements. For example, in 2024, capital expenditures reached $690 million, with projections for 2025 between $630 million and $690 million, aimed at increasing patient bed capacity and enhancing overall facility infrastructure.
The company also incurs costs for regulatory compliance, licensing, and quality improvement initiatives, which are critical for maintaining operational standards and patient safety. These expenses ensure adherence to industry regulations and accreditations, underpinning Acadia's commitment to high-quality care delivery.
| Cost Category | Description | 2024 Impact/Focus |
| Staff Costs | Salaries, wages, benefits for ~25,500 employees | Significant driver of operational expenses; focus on talent retention. |
| Facility Operations & Maintenance | Utilities, rent/mortgage, repairs, environmental services for 270 facilities | Essential for safety, compliance, and functionality; ongoing upkeep is critical. |
| Medical Supplies & Pharmaceuticals | Consumables, medications (incl. MAT programs), specialized equipment | Continued growth in sector spending; efficient procurement is key for cost control. |
| Capital Expenditures | New facilities, expansions, acquisitions, infrastructure improvements | $690 million spent in 2024; $630-$690 million projected for 2025 to add beds and improve infrastructure. |
| Regulatory Compliance & Quality | Licensing, accreditation, quality improvement programs, audits | Ensures adherence to standards, safety, and high-quality care delivery. |
Revenue Streams
Acadia Healthcare's primary revenue engine is driven by insurance reimbursements, both from private commercial insurers and government payers like Medicare and Medicaid. These reimbursements are crucial as they directly fund the inpatient, residential, and outpatient behavioral health services Acadia offers to its patients.
For instance, in 2024, Acadia Healthcare's financial health is significantly influenced by the volume of patients utilizing their services and the prevailing reimbursement rates set by these insurance entities. Fluctuations in these rates or patient census can directly impact the company's top-line performance.
Acadia Healthcare also generates revenue directly from patients through co-pays, deductibles, and private pay arrangements. This means individuals pay a portion of their healthcare costs out-of-pocket, either because their insurance requires it or because they opt for services not covered by insurance plans. For instance, in 2023, the average deductible for employer-sponsored health plans in the US was around $1,700 for individuals, highlighting the potential for patient co-payments and deductibles to contribute significantly to provider revenue.
Acadia Healthcare's revenue is significantly boosted by specialized program fees. These fees are generated from intensive treatment offerings for conditions like eating disorders and specific substance use disorders. For instance, in 2024, Acadia's specialized behavioral health services, which encompass these intensive programs, continued to be a key revenue driver, reflecting the demand for targeted therapeutic interventions.
Revenue from New and Expanded Facilities
Acadia's revenue is significantly boosted by its strategic expansion of healthcare facilities. This includes building new de novo locations, adding capacity to existing sites, and forming joint ventures. These initiatives are designed to capture new patient volumes and generate associated revenue streams, fueling the company's growth trajectory.
This strategy has proven to be a key growth engine for Acadia. In 2024, the company reported substantial revenue increases directly attributable to these facility expansions. Looking ahead to 2025, this trend is expected to continue, further solidifying its market position.
- De Novo Facilities: Opening new locations directly adds patient capacity and revenue generation potential.
- Facility Expansions: Increasing bed count in existing facilities allows for higher patient throughput and revenue.
- Joint Ventures: Partnerships enable shared investment and operational costs, accelerating market penetration and revenue growth.
- 2024 Performance: Acadia saw considerable revenue uplift from these expansion efforts throughout the year.
Ancillary Services and Value-Added Offerings
Acadia can generate revenue through ancillary services that go beyond core treatment. These might include specialized therapy groups, comprehensive aftercare planning, or other offerings that enhance a patient's recovery journey. For instance, in 2024, the mental health and substance abuse treatment sector saw a growing demand for such supplementary services, with some providers reporting up to 15% of their total revenue coming from these value-added programs.
These additional services, while perhaps smaller in individual contribution, are crucial for diversifying Acadia's revenue streams. They also play a significant role in improving patient satisfaction and outcomes, which can lead to better retention and referrals. In 2023, patient satisfaction scores for facilities offering robust ancillary services were, on average, 10% higher than those without.
- Specialized Therapy Groups: Offering niche groups like trauma-informed yoga or mindfulness sessions can attract specific patient needs and generate fees.
- Aftercare Planning Services: Providing detailed post-discharge support, including relapse prevention strategies and community resource connections, adds significant value.
- Wellness Programs: Complementary services such as nutritional counseling or fitness programs can be offered as premium add-ons.
- Educational Workshops: Sessions for families or patients on managing mental health conditions or addiction recovery can be a distinct revenue source.
Acadia Healthcare's revenue is primarily derived from reimbursements by private insurance companies and government programs like Medicare and Medicaid for its behavioral health services. In 2024, the company's financial performance is closely tied to patient volumes and the reimbursement rates established by these payers.
Direct patient payments, including co-pays and deductibles, also contribute to Acadia's revenue. For instance, in 2023, average deductibles for employer-sponsored health plans were around $1,700, indicating the potential for patient out-of-pocket contributions.
Specialized program fees for intensive treatments, such as those for eating disorders and substance use disorders, represent another significant revenue stream. These targeted interventions continue to be a key driver of income in 2024 due to high demand.
Acadia also generates revenue through ancillary services like specialized therapy groups and aftercare planning, which enhance patient recovery and diversify income. In 2024, the mental health sector saw a growing demand for these value-added programs, with some providers earning up to 15% of revenue from them.
| Revenue Source | Description | 2024 Impact/Trend |
| Insurance Reimbursements | Payments from private insurers, Medicare, and Medicaid. | Core revenue driver; sensitive to rates and patient census. |
| Patient Payments | Co-pays, deductibles, and private pay for services. | Contributes directly, influenced by insurance plan structures. |
| Specialized Program Fees | Fees for intensive treatments (e.g., eating disorders, substance abuse). | Key growth area due to demand for targeted care. |
| Ancillary Services | Value-added services like specialized therapy groups and aftercare. | Diversifies revenue and improves patient outcomes. |
Business Model Canvas Data Sources
The Acadia Business Model Canvas is informed by a combination of internal financial data, comprehensive market research, and expert strategic analysis. These diverse sources ensure each component of the canvas is robust and reflective of current business realities.