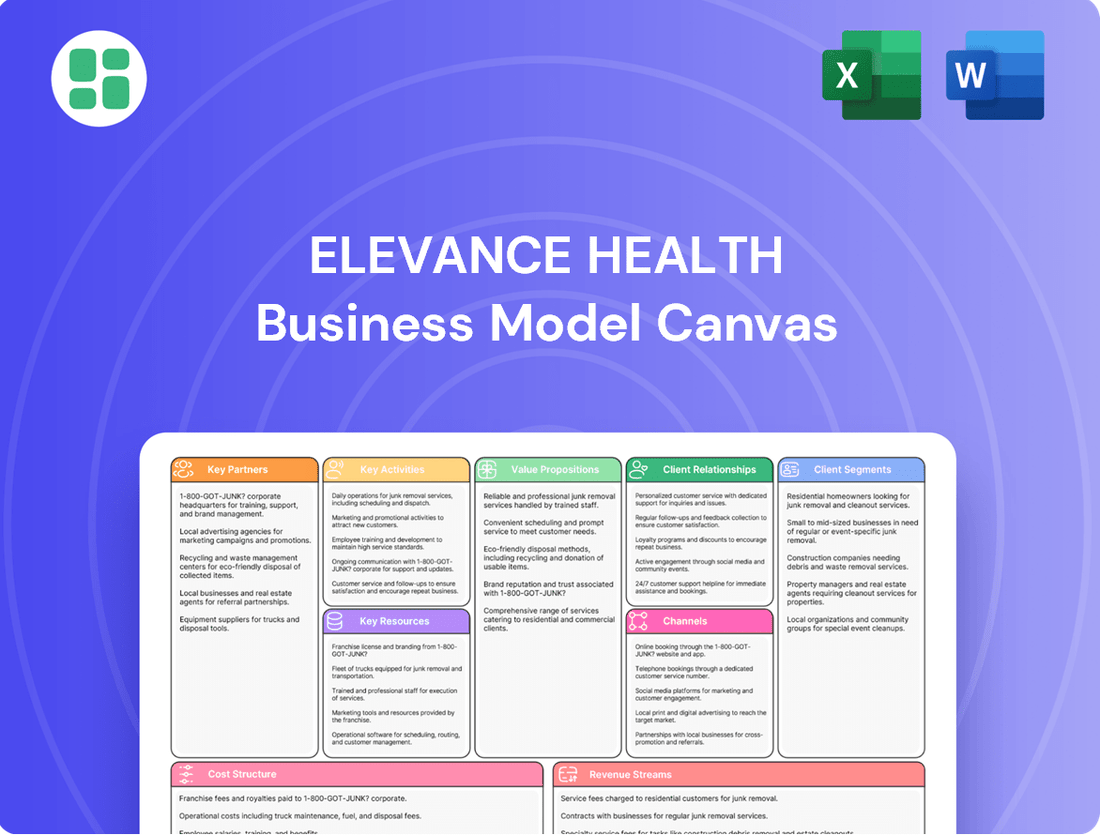
Elevance Health Business Model Canvas
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
Elevance Health Bundle
Unlock the strategic blueprint behind Elevance Health's innovative approach to healthcare. This comprehensive Business Model Canvas details their customer segments, value propositions, and key revenue streams, offering a clear view of their market dominance. Discover how Elevance Health effectively manages its cost structure and leverages key resources to deliver integrated health solutions.
Partnerships
Elevance Health cultivates deep relationships with a vast array of healthcare providers and integrated health systems. These partnerships are fundamental to their ability to offer members a broad spectrum of medical services and manage patient care effectively. As of 2024, Elevance Health's network includes a significant number of hospitals and physician groups across its operating regions, enabling them to deliver coordinated care and pursue value-based reimbursement strategies.
Elevance Health actively collaborates with technology and digital health companies to bolster its digital infrastructure. These partnerships are crucial for integrating advanced technologies like artificial intelligence and predictive analytics into its service offerings.
These alliances are instrumental in developing and enhancing platforms such as the Sydney Health app. This app leverages data-driven insights to personalize member experiences, streamline administrative processes, and ultimately improve health outcomes for Elevance Health’s members.
In 2024, Elevance Health continued to invest in digital transformation, with technology partnerships playing a key role. For instance, the company’s focus on AI and machine learning in areas like claims processing and care management aims to drive efficiency and better patient care, reflecting a strategic commitment to digital innovation.
Elevance Health partners with pharmaceutical companies to manage prescription drug expenses and ensure member access to medications. This collaboration is crucial for maintaining competitive drug pricing and developing effective formularies.
Through its PBM, CarelonRx, Elevance Health actively negotiates drug prices, aiming to reduce costs for its members and the company. In 2024, PBMs played a significant role in the healthcare landscape, with industry reports indicating substantial savings generated through these negotiations.
Government Entities and Community Organizations
Elevance Health's key partnerships with government entities are crucial for its operational success, particularly in managing Medicare and Medicaid programs. These government contracts are a significant driver of revenue, as these programs serve vast customer bases. For instance, in 2024, government health programs continue to be a cornerstone of the health insurance landscape, with millions relying on them for care.
Collaborations with non-profit and community organizations are also vital. These partnerships allow Elevance Health to address social determinants of health, offering support for essential needs like housing and food security to vulnerable populations. This holistic approach enhances member well-being and strengthens community ties.
- Government Contracts: Essential for administering Medicare and Medicaid, representing substantial customer segments and revenue streams.
- Community Engagement: Partnerships with non-profits and community groups address social determinants of health, improving member outcomes.
- Program Reach: These collaborations expand Elevance Health's ability to serve diverse and often underserved populations effectively.
Employers and Brokers
Elevance Health collaborates closely with employers, offering customized group health insurance and administrative services designed for businesses of all sizes. This symbiotic relationship ensures that companies can provide comprehensive benefits to their workforce.
Brokers and consultants play a crucial role in Elevance Health's distribution strategy. These intermediaries are essential for reaching a wider array of employer and individual clients, effectively expanding Elevance Health's market penetration.
- Employer Partnerships: Elevance Health serves over 100,000 employers across the nation, demonstrating the breadth of its reach in the employer market.
- Broker Network: In 2024, Elevance Health continued to leverage its extensive network of brokers and consultants, which is critical for distributing its diverse health plan offerings.
- Tailored Solutions: The company emphasizes its ability to provide bespoke benefit solutions, catering to the unique needs of each employer, from small businesses to large corporations.
- Market Access: Partnerships with brokers are key to accessing both the commercial group market and individual and family plans, driving significant membership growth.
Elevance Health's key partnerships extend to pharmaceutical companies and pharmacy benefit managers (PBMs) like CarelonRx. These collaborations are vital for managing prescription drug costs and ensuring members have access to necessary medications. In 2024, the strategic negotiation of drug prices through PBMs remained a critical component for cost containment and formulary management.
| Partner Type | Role | Impact |
| Healthcare Providers & Systems | Service Delivery & Care Coordination | Broad member access, value-based care |
| Technology Companies | Digital Infrastructure & Innovation | Enhanced member experience, AI integration |
| Pharmaceutical Companies & PBMs | Drug Access & Cost Management | Competitive pricing, effective formularies |
What is included in the product
This Elevance Health Business Model Canvas outlines their strategy for providing health and well-being solutions, focusing on diverse customer segments like employers, individuals, and government programs.
It details their value propositions, including personalized care and cost-effective health plans, delivered through integrated digital platforms and a vast provider network.
Elevance Health's Business Model Canvas acts as a pain point reliever by offering a clear, one-page snapshot of their complex healthcare operations, simplifying understanding and strategic alignment.
It provides a structured framework to pinpoint and address inefficiencies within their value chain, thereby reducing operational friction and improving member outcomes.
Activities
Elevance Health actively develops and manages a wide array of health insurance products, encompassing traditional HMOs and PPOs, alongside government-sponsored Medicare Advantage and Medicaid plans. This dynamic process involves thorough market research to understand consumer preferences and rigorous actuarial analysis to ensure financial viability. In 2024, Elevance Health's commitment to innovation in product design is crucial for navigating the complex healthcare landscape and addressing diverse member needs.
Elevance Health's key activities heavily revolve around the efficient processing of medical, pharmacy, and behavioral health claims. This operational backbone ensures that members receive timely access to care by facilitating payments to healthcare providers.
Managing a vast network of healthcare providers is equally crucial. This involves rigorous credentialing processes, negotiating favorable contracts, and ensuring prompt payment cycles to maintain the quality and accessibility of the care delivery system for its members.
In 2023, Elevance Health reported processing billions of claims, underscoring the scale of this critical function. The company's provider network encompasses hundreds of thousands of physicians and facilities, demonstrating the extensive reach required for effective network administration.
Elevance Health's core activities center on robust care management, encompassing both physical and behavioral health services, alongside comprehensive pharmacy solutions. This integrated approach is designed to proactively improve member health outcomes through personalized care coordination and targeted interventions.
The company actively implements programs that address the multifaceted drivers of health, including social determinants, to ensure holistic well-being for its members. In 2023, Elevance Health reported a significant focus on these areas, aiming to reduce healthcare costs and enhance patient experiences.
Digital Transformation and Technology Innovation
Elevance Health actively invests in and deploys advanced digital solutions, including artificial intelligence and data analytics. These technologies are crucial for improving how the company operates, tailoring experiences for its members, and expanding telehealth services. For instance, in 2024, the company continued to refine its Sydney Health platform, a key digital touchpoint for members.
Automating core business processes is another vital activity. This focus on technology innovation helps streamline operations, reduce costs, and enhance the speed and accuracy of service delivery. Elevance Health’s commitment to digital transformation underpins its strategy to deliver better health outcomes and a more personalized member journey.
- Digital Solutions Deployment: Continued investment in AI and data analytics to optimize operations and personalize member experiences.
- Platform Development: Ongoing enhancement of digital platforms like Sydney Health to serve as a central member engagement tool.
- Process Automation: Automation of core business processes to drive efficiency and improve service delivery.
- Telehealth Expansion: Leveraging technology to broaden access to virtual care options for members.
Regulatory Compliance and Risk Management
Elevance Health's key activities include rigorously ensuring all its operations comply with the intricate web of healthcare regulations, a critical component for maintaining trust and operational legitimacy. This involves constant vigilance over evolving laws and the implementation of comprehensive frameworks to guarantee adherence.
Managing significant financial risks, such as volatile medical cost trends and the complexities of underwriting, is another core activity. Elevance Health actively monitors these factors to maintain financial stability and profitability in a dynamic market. For instance, in 2024, the company reported a medical cost ratio that reflects ongoing efforts to manage these trends effectively.
- Regulatory Adherence: Actively monitoring and adapting to changes in healthcare legislation, including HIPAA, ACA, and state-specific mandates.
- Financial Risk Mitigation: Implementing strategies to manage medical cost trends, including provider negotiations and value-based care initiatives.
- Underwriting Excellence: Utilizing data analytics to refine underwriting processes, ensuring accurate risk assessment and pricing.
- Compliance Frameworks: Developing and maintaining robust internal controls and compliance programs to prevent violations and associated penalties.
Elevance Health's key activities center on developing and managing a diverse range of health insurance products, from traditional plans to government-sponsored options like Medicare Advantage. This involves deep market research and actuarial analysis to ensure products meet member needs and financial viability. In 2024, innovation in product design remains paramount for navigating the complex healthcare landscape.
Core operations include the efficient processing of billions of claims for medical, pharmacy, and behavioral health services, ensuring timely access to care and provider payments. Managing an extensive network of hundreds of thousands of physicians and facilities through credentialing and contract negotiation is also vital for delivering accessible, quality care.
Proactive care management, covering both physical and behavioral health, alongside comprehensive pharmacy solutions, aims to improve member health outcomes. This includes addressing social determinants of health to foster holistic well-being, a focus that Elevance Health intensified in 2023 to reduce costs and enhance patient experiences.
Elevance Health actively deploys advanced digital solutions, including AI and data analytics, to optimize operations and personalize member experiences, exemplified by the ongoing refinement of its Sydney Health platform in 2024. Automating business processes further drives efficiency and service delivery speed.
Ensuring strict adherence to healthcare regulations and managing financial risks, such as volatile medical cost trends, are critical ongoing activities. Elevance Health utilizes data analytics for underwriting excellence and implements strategies to mitigate financial risks, as reflected in its 2024 medical cost ratio management.
What You See Is What You Get
Business Model Canvas
The Elevance Health Business Model Canvas you are previewing is the exact document you will receive upon purchase. This comprehensive overview outlines key aspects of Elevance Health's operations, including customer segments, value propositions, channels, and revenue streams. Rest assured, what you see is the complete, ready-to-use business model, offering a transparent and accurate representation of the final deliverable.
Resources
Elevance Health leverages an extensive provider network, a cornerstone of its business model. This network encompasses a wide array of healthcare facilities, including hospitals, physician groups, and specialized care centers, strategically positioned across the nation. By the end of 2023, Elevance Health served over 120 million people, underscoring the sheer scale and reach of its provider relationships.
This vast network is crucial for delivering accessible and comprehensive healthcare services to its diverse membership. It allows Elevance Health to offer a broad spectrum of medical treatments and specialties, ensuring members can find the care they need close to home. The strength of these relationships is vital for managing costs and ensuring quality outcomes for patients.
Elevance Health's significant investments in advanced technology and data infrastructure are foundational. In 2024, the company continued to prioritize its IT backbone, including substantial allocations to cloud computing, artificial intelligence (AI), and big data analytics. These capabilities are not just operational tools; they are critical resources that drive efficiency and innovation across the business.
These technological advancements directly support key operational functions. For instance, AI and big data analytics are instrumental in streamlining claims processing, which is a core activity for any health insurer. Furthermore, these systems enable more personalized member engagement strategies and enhance the detection of fraudulent activities, safeguarding company resources and improving member experience.
The company's commitment to data-driven decision-making is powered by this robust infrastructure. By leveraging AI and advanced analytics, Elevance Health can gain deeper insights into member health trends, optimize care pathways, and identify opportunities for cost savings. This analytical prowess is crucial for navigating the complex healthcare landscape and maintaining a competitive edge.
Elevance Health’s business model hinges on its skilled workforce, including actuaries, medical professionals, and data scientists. In 2024, the company continued to invest in these human capital resources, recognizing their critical role in developing innovative health plans and delivering exceptional member services.
The expertise of Elevance Health’s employees directly impacts product development and strategic execution. Their collective knowledge allows the company to navigate complex healthcare regulations and market dynamics, ensuring competitive offerings and efficient operations.
Financial Capital and Reserves
Elevance Health maintains substantial financial capital and reserves, a cornerstone for its operational stability and capacity to manage claims. This financial strength is critical for ensuring the company can meet its obligations to policyholders and invest in future growth initiatives.
As of the first quarter of 2024, Elevance Health reported total assets of approximately $154.4 billion, underscoring its significant financial resources. This robust capital base enables the company to absorb market fluctuations, pursue strategic acquisitions, and drive innovation in healthcare services.
- Financial Stability: Strong reserves allow Elevance Health to confidently cover current and future claims, ensuring policyholder trust and operational continuity.
- Growth and Investment: Ample capital fuels sustained growth, facilitates strategic acquisitions, and supports investment in new technologies and service offerings.
- Market Resilience: A substantial financial cushion enhances the company's ability to navigate economic downturns and industry-specific challenges.
- Shareholder Value: Financial strength supports consistent dividend payments and share buybacks, contributing to enhanced shareholder returns.
Intellectual Property and Proprietary Programs
Elevance Health's intellectual property and proprietary programs are cornerstones of its business model, offering significant competitive advantages. These include unique health plan designs tailored to diverse member needs and sophisticated care management programs, such as those operated under the Carelon brand. These specialized programs are designed to improve health outcomes and manage costs effectively. In 2024, Elevance Health continued to invest in these areas, recognizing their critical role in differentiating its offerings.
The company's digital health platforms, notably the Sydney Health app, represent another vital piece of intellectual property. These platforms provide members with convenient access to health information, services, and personalized support. Coupled with advanced data analytics models, these digital tools enable Elevance Health to gain deeper insights into member behavior and healthcare trends, driving more effective and personalized interventions. This technological infrastructure is key to their strategy of delivering integrated, whole-health solutions.
These proprietary resources are not merely technological assets but are integral to Elevance Health's value proposition. They allow the company to:
- Develop differentiated health insurance products and services.
- Enhance member engagement and health outcomes through personalized care.
- Leverage data analytics for operational efficiency and strategic decision-making.
- Strengthen its market position against competitors.
Elevance Health's key resources include its expansive provider network, advanced technology and data infrastructure, a skilled workforce, substantial financial capital, and proprietary intellectual property. These elements collectively underpin the company's ability to deliver comprehensive healthcare solutions and maintain a competitive edge in the market.
| Key Resource | Description | 2023/2024 Data Point |
| Provider Network | Nationwide network of healthcare facilities and professionals. | Served over 120 million people by end of 2023. |
| Technology & Data Infrastructure | Investments in AI, cloud computing, and big data analytics. | Continued prioritization of IT backbone in 2024. |
| Human Capital | Skilled workforce including actuaries, medical professionals, and data scientists. | Continued investment in human capital resources in 2024. |
| Financial Capital | Substantial financial reserves and assets. | Approximately $154.4 billion in total assets as of Q1 2024. |
| Intellectual Property | Proprietary health plan designs, care management programs, and digital platforms like Sydney Health. | Continued investment in differentiating offerings in 2024. |
Value Propositions
Elevance Health offers a broad spectrum of health insurance options, encompassing HMOs, PPOs, Medicare, and Medicaid. This extensive portfolio serves individuals, families, and employers, ensuring a fit for varied health requirements and financial capacities.
These plans deliver comprehensive medical benefits, designed to address a wide range of health needs and budgets. For instance, in 2023, Elevance Health served over 100 million people, demonstrating its significant reach in providing diverse health coverage solutions.
Elevance Health's value proposition centers on enhancing health outcomes through a comprehensive, whole-person care model. This involves seamlessly integrating physical, behavioral, and social health services, recognizing that a person's well-being is influenced by a multitude of factors beyond just medical treatment.
The company actively employs care management programs designed to support members across their health journey. For instance, in 2023, Elevance Health reported significant engagement in its care management initiatives, with millions of members benefiting from personalized support designed to improve their overall health and reduce preventable healthcare costs.
Elevance Health offers members extensive access to a wide array of healthcare providers, fostering convenience and choice in their medical care journey. This broad network is a cornerstone of their value proposition, ensuring individuals can find the right care when and where they need it.
The company actively cultivates partnerships with high-quality providers, a commitment that directly translates into an enhanced care experience for its members. This focus on quality assurance means members can expect a higher standard of medical attention and service.
For instance, in 2024, Elevance Health continued to expand its network, reporting that its affiliated providers served approximately 119 million people. This scale underscores the breadth of access available to its members.
Cost Management and Affordability
Elevance Health's commitment to cost management and affordability is a cornerstone of its value proposition. By utilizing its significant scale, the company can negotiate more favorable rates with healthcare providers, directly impacting the cost of care for its members and the employers who offer its plans. This negotiating power is crucial in keeping premiums and out-of-pocket expenses manageable.
A key strategy Elevance employs is the implementation of value-based care arrangements. These models incentivize providers to focus on quality outcomes and cost efficiency rather than the volume of services. This shift helps to reduce unnecessary procedures and improve patient health, ultimately lowering overall healthcare expenditures. For example, in 2023, Elevance Health reported that its value-based care initiatives contributed to significant savings and improved quality metrics across its network.
- Leveraging Scale for Negotiation: Elevance Health's large membership base allows for stronger bargaining power with hospitals and pharmaceutical companies, leading to reduced prices.
- Value-Based Care Implementation: Shifting from fee-for-service to value-based payment models incentivizes providers to deliver efficient, high-quality care, thereby controlling costs.
- Focus on Preventative Care: Investing in preventative services and chronic disease management programs helps avoid more expensive treatments down the line.
- Operational Efficiencies: Streamlining administrative processes and utilizing technology further contribute to lowering the overall cost of delivering healthcare services.
Personalized Digital Engagement and Support
Elevance Health leverages digital platforms, notably the Sydney Health app, to deliver highly personalized health engagement and support. This digital ecosystem provides members with tailored health recommendations, seamless access to telehealth services, and streamlined administrative interactions, fostering a proactive approach to well-being.
The Sydney Health app, a cornerstone of Elevance Health's digital strategy, offers a comprehensive suite of tools designed to empower members. By integrating personalized insights with convenient access to care, the platform aims to improve health outcomes and member satisfaction. In 2024, Elevance Health reported significant growth in digital engagement, with millions of members actively using its digital tools for health management and care access.
- Personalized Health Recommendations: AI-driven insights guide members toward preventative care and healthier lifestyle choices.
- Telehealth Accessibility: Convenient virtual consultations connect members with healthcare providers, improving access to care.
- Simplified Interactions: Digital tools streamline benefit navigation, claims processing, and appointment scheduling.
- Proactive Health Management: Encourages members to take an active role in their health journey through accessible digital resources.
Elevance Health's value proposition is built on delivering comprehensive, whole-person care by integrating physical, behavioral, and social health services. This holistic approach aims to improve member well-being beyond traditional medical treatment.
The company champions preventative care and robust care management programs, guiding members through their health journeys. In 2023, millions of members benefited from personalized support, demonstrating a commitment to improving health outcomes and reducing avoidable costs.
Elevance Health provides extensive access to a broad network of high-quality healthcare providers, ensuring members can find convenient and appropriate care. By the end of 2024, its affiliated providers served approximately 119 million people, highlighting the vastness of its network.
The company focuses on affordability and cost management through its scale, enabling favorable negotiations with providers, which helps manage premiums and out-of-pocket expenses for members and employers. Its value-based care initiatives in 2023 showed success in improving quality and generating savings.
Customer Relationships
Elevance Health leverages digital channels, notably the Sydney Health app, to foster personalized customer relationships. This platform provides members with tailored health insights and streamlined self-service capabilities, enhancing their ability to manage benefits and access care resources efficiently.
Elevance Health prioritizes dedicated customer service, operating extensive call centers to assist members with claims, benefits, and healthcare navigation. In 2024, the company continued to invest in its advocacy solutions, aiming to resolve member queries efficiently and improve overall satisfaction.
This focus on personalized support is crucial for retaining members and fostering loyalty within their diverse customer base. By addressing individual needs promptly, Elevance Health strives to achieve high satisfaction rates, a key component of their customer relationship strategy.
Elevance Health cultivates strong customer relationships through dedicated care management and health coaching. These programs offer personalized guidance, helping members navigate their health needs and achieve better wellness. This proactive approach builds trust and encourages long-term engagement.
In 2024, Elevance Health continued to emphasize these member-centric services. Their focus on behavioral health support and tailored health coaching aims to improve member satisfaction and retention. By actively assisting individuals in their health journeys, Elevance fosters loyalty and demonstrates a commitment to improved health outcomes.
Community Engagement and Support Programs
Elevance Health actively fosters community engagement through programs that go beyond traditional healthcare. These initiatives tackle crucial social determinants of health, aiming to improve overall well-being.
In 2024, Elevance Health continued its focus on addressing food insecurity and housing stability. For instance, their collaborations with local food banks and housing assistance programs provided tangible support to vulnerable populations, reinforcing their commitment to holistic health.
- Community Health Initiatives: Elevance Health invests in programs addressing social determinants of health, such as food security and housing, in 2024.
- Holistic Well-being Focus: These efforts underscore a dedication to the overall health and well-being of individuals and communities.
- Strengthened Community Ties: By actively participating in and supporting community-based solutions, Elevance Health builds stronger relationships and trust.
Transparent Communication and Reporting
Elevance Health prioritizes transparent communication to foster trust with its members. This involves clearly outlining plan benefits, associated costs, and adherence to regulatory requirements. For instance, in 2024, the company continued its commitment to providing accessible information through various channels, ensuring members understand their healthcare options and responsibilities.
Regular updates and informative content are key to keeping members engaged. Elevance Health utilizes newsletters, online portals, and direct communications to share important plan changes, wellness tips, and relevant health news. This proactive approach helps members make informed decisions about their health and healthcare spending.
- Clear Plan Details: Providing upfront information on deductibles, copays, and out-of-pocket maximums.
- Regulatory Adherence: Ensuring all communications meet federal and state compliance standards.
- Member Engagement: Utilizing newsletters and digital platforms for ongoing updates and educational content.
- Cost Transparency: Offering tools and resources to help members understand and manage healthcare expenses.
Elevance Health's customer relationship strategy centers on personalized digital engagement, robust customer service, and community-focused initiatives. The Sydney Health app serves as a key platform for tailored insights and self-service, while extensive call centers handle member inquiries. In 2024, the company's investment in advocacy solutions and member-centric services like health coaching aimed to boost satisfaction and retention.
| Customer Relationship Aspect | Description | 2024 Focus/Data Point |
|---|---|---|
| Digital Engagement | Personalized insights and self-service via Sydney Health app | Continued investment in app features for enhanced member experience. |
| Customer Service | Extensive call centers for claims, benefits, and navigation support | Focus on efficient query resolution through advocacy solutions. |
| Health Coaching & Care Management | Personalized guidance for wellness and health needs | Emphasis on behavioral health support and tailored coaching for improved outcomes. |
| Community Initiatives | Addressing social determinants of health (food security, housing) | Collaborations with local organizations to provide tangible support. |
| Transparency & Communication | Clear benefit details, costs, and regulatory adherence | Ongoing commitment to accessible information via newsletters and portals. |
Channels
Elevance Health leverages its direct sales and online platforms to connect with individual consumers. Their websites and dedicated enrollment portals offer a streamlined experience for browsing, comparing, and purchasing health insurance plans. This digital approach ensures convenient, 24/7 access for customers seeking coverage.
In 2024, Elevance Health continued to see significant engagement through these digital channels. While specific enrollment figures for direct online sales are proprietary, the broader trend in the health insurance market indicates a strong preference for digital self-service options. For instance, industry reports from 2023 showed that over 60% of health insurance shoppers utilized online tools to research and select plans, a trend expected to grow.
Elevance Health extensively utilizes employer partnerships as a core channel, offering group health insurance plans that reach millions of individuals. In 2024, this strategy continued to be a cornerstone of their market penetration, providing access to a broad and stable customer base.
Independent insurance brokers and consultants are vital intermediaries, facilitating the distribution of Elevance Health's diverse plan offerings to businesses of all sizes and individual consumers. These networks are crucial for navigating complex benefit choices and ensuring plan suitability.
Elevance Health leverages government programs like Medicare and Medicaid as crucial channels, directly serving millions of beneficiaries. In 2024, these government contracts represent a substantial portion of Elevance's revenue, underscoring their importance in the company's business model. For instance, Medicare Advantage enrollment alone saw continued growth, with millions of Americans choosing these plans for their healthcare needs.
Healthcare Provider Networks
Elevance Health's extensive network of affiliated healthcare providers acts as a critical channel, enabling members to access essential medical care and services. This robust network, comprising doctors, hospitals, and other facilities, is fundamental to delivering on Elevance Health's value proposition of accessible and coordinated care.
The strategic importance of these provider networks is underscored by Elevance Health's significant investments. For instance, in 2024, the company continued to focus on strengthening these relationships, aiming to improve patient outcomes and manage costs effectively through integrated care models. This approach ensures that members can readily find and utilize in-network services, a key driver of member satisfaction and retention.
- Provider Network Size: Elevance Health serves millions of members through its broad network, which includes a substantial number of physicians and hospitals across its operating states.
- Value-Based Care: The company actively promotes value-based care arrangements within its provider networks, aligning incentives for quality outcomes and cost efficiency.
- Digital Integration: Efforts in 2024 focused on enhancing digital tools for members to easily find and connect with in-network providers, streamlining the care access experience.
- Geographic Reach: The localized presence of these provider networks is vital for ensuring members have convenient access to care in their communities.
Digital Health Applications and Telehealth Services
Digital health applications and telehealth services are pivotal channels for Elevance Health, exemplified by the Sydney Health app. This platform facilitates member engagement, offering virtual consultations and personalized health management solutions. In 2024, telehealth adoption continued its strong upward trend, with many health insurers reporting significant increases in virtual visits compared to pre-pandemic levels, improving accessibility and convenience for millions of members.
- Sydney Health App: A key digital touchpoint for member interaction and service access.
- Telehealth Integration: Enables virtual consultations, enhancing care delivery convenience.
- Member Engagement: Digital channels foster proactive health management and personalized experiences.
- Accessibility & Convenience: These services remove geographical and time barriers to healthcare.
Elevance Health utilizes a multi-faceted approach to reach its diverse customer base. Direct-to-consumer sales through online platforms and a dedicated sales force cater to individuals seeking health insurance. Employer-sponsored plans remain a significant channel, leveraging corporate relationships to provide coverage to millions of employees. Furthermore, partnerships with independent brokers and consultants extend the reach of Elevance's offerings to businesses and individuals alike.
Government programs, particularly Medicare and Medicaid, represent substantial distribution channels for Elevance Health, serving millions of beneficiaries. The company's extensive network of affiliated healthcare providers is a critical channel, ensuring members have access to care and facilitating integrated health management. Digital health applications and telehealth services, such as the Sydney Health app, are increasingly important for member engagement and convenient access to care.
| Channel | Description | 2024 Relevance/Data Point |
|---|---|---|
| Direct Sales & Online Platforms | Website enrollment, dedicated portals | Continued strong digital engagement, mirroring 2023 trend of 60%+ online shoppers. |
| Employer Partnerships | Group health insurance plans | Cornerstone for market penetration, providing stable customer base. |
| Brokers & Consultants | Intermediaries for plan distribution | Vital for navigating complex choices for businesses and individuals. |
| Government Programs (Medicare/Medicaid) | Serving beneficiaries directly | Substantial revenue source, with continued growth in Medicare Advantage enrollment. |
| Provider Networks | Access to doctors, hospitals, facilities | Fundamental to delivering accessible care; focus on strengthening relationships in 2024. |
| Digital Health & Telehealth | Sydney Health app, virtual consultations | Strong upward trend in telehealth adoption, enhancing accessibility. |
Customer Segments
Elevance Health directly serves individuals and families by offering a wide array of health insurance plans. These plans are accessible through various channels, including the Affordable Care Act (ACA) marketplaces, providing options for those needing coverage outside of employer-sponsored benefits.
The company's offerings are designed to meet a broad spectrum of health requirements and financial capacities. For instance, in 2024, Elevance Health continued to expand its presence on ACA exchanges in numerous states, aiming to provide more choices and competitive pricing to consumers navigating the individual market.
Employer groups, spanning small, medium, and large businesses, represent a core customer segment for Elevance Health. They rely on Elevance for comprehensive group health insurance plans and administrative services only (ASO) arrangements, covering a broad spectrum of corporate and business clients.
In 2024, Elevance Health continued to serve a vast network of employers, with their employer-sponsored insurance plans being a primary driver of revenue. The company's ability to tailor offerings to the diverse needs of businesses, from startups to Fortune 500 companies, solidifies this segment's importance.
Medicare beneficiaries, encompassing seniors and other eligible individuals, represent a core customer segment for Elevance Health. The company offers a range of Medicare Advantage and Medicare Supplement plans designed to meet the diverse healthcare needs of this population. In 2024, Elevance Health continued its strategic focus on expanding its reach within this vital market.
Elevance Health is actively pursuing growth opportunities within the Medicare Advantage space, including securing group Medicare Advantage contracts. This strategic push aims to capture a larger share of the burgeoning senior healthcare market, reflecting the segment's importance to the company's overall business model. The company's performance in this segment is closely watched by investors and industry analysts.
Medicaid Beneficiaries
Elevance Health serves Medicaid beneficiaries across multiple states, acting as a crucial administrator for government-funded healthcare programs. This involves providing essential medical coverage to individuals and families with low incomes, as well as those with disabilities, often addressing multifaceted health and social challenges.
In 2024, Elevance Health's Medicaid business continued to be a significant driver of its overall revenue. For instance, their Medicaid membership reached over 5 million individuals by the end of the first quarter of 2024, reflecting the substantial scale of their operations in this segment.
- Medicaid Administration: Elevance Health manages state-specific Medicaid programs, ensuring access to care for vulnerable populations.
- Complex Needs Management: The company focuses on supporting beneficiaries with complex health and social requirements, aiming for improved health outcomes.
- Membership Growth: As of Q1 2024, Elevance Health reported a substantial Medicaid membership base exceeding 5 million individuals.
Federal Employees
Elevance Health extends its services to federal employees through dedicated health benefit programs, showcasing its involvement in government-administered health coverage. This segment necessitates strict compliance with federal regulations and program specifications.
For instance, in 2024, federal employees were offered various health insurance options under the Federal Employees Health Benefits (FEHB) Program, with Elevance Health, through its Blue Cross Blue Shield plans, being a significant provider in many regions. These plans often include comprehensive medical, dental, and vision coverage.
- Federal Employees Health Benefits (FEHB) Program: A cornerstone of healthcare for civilian federal employees and annuitants.
- Elevance Health's Role: Provides coverage through its various Blue Cross Blue Shield affiliated health plans across numerous states.
- Compliance Requirements: Adherence to specific federal guidelines, benefit structures, and enrollment periods mandated by the Office of Personnel Management (OPM).
- Market Penetration: In 2024, Elevance Health continued to be a major player in the FEHB market, serving hundreds of thousands of federal employees and their families.
Elevance Health's customer base is diverse, encompassing individuals and families seeking coverage through ACA marketplaces, demonstrating a commitment to accessible healthcare. The company also serves a substantial number of employer groups, from small businesses to large corporations, offering tailored group health insurance and administrative services. Furthermore, Elevance Health is a major provider for Medicare beneficiaries, offering Advantage and Supplement plans, and plays a critical role in administering state Medicaid programs, serving millions of low-income individuals and families.
| Customer Segment | Key Offerings | 2024 Data/Focus |
|---|---|---|
| Individuals & Families | ACA Marketplace plans | Expanded presence on ACA exchanges, offering more choices and competitive pricing. |
| Employer Groups | Group health insurance, ASO arrangements | Serves small, medium, and large businesses; plans tailored to diverse needs. |
| Medicare Beneficiaries | Medicare Advantage, Medicare Supplement plans | Strategic focus on expanding reach and securing group Medicare Advantage contracts. |
| Medicaid Beneficiaries | State Medicaid program administration | Over 5 million individuals in Medicaid membership as of Q1 2024; focus on complex needs management. |
| Federal Employees | FEHB Program plans | Major provider through Blue Cross Blue Shield affiliations, serving hundreds of thousands. |
Cost Structure
Medical benefit expenses represent the most significant cost for Elevance Health, encompassing payments made to healthcare providers like hospitals and doctors for services rendered to members. These expenses are intrinsically linked to how often members use healthcare services and the prevailing trends in medical costs.
In 2024, for instance, Elevance Health reported that its total medical costs were a substantial portion of its revenue, reflecting the direct impact of member health needs and the cost of care delivery. The company's ability to manage these costs effectively through network negotiations and care management programs is crucial for its profitability.
Elevance Health faces significant administrative and operating expenses, a core component of its cost structure. These costs encompass essential functions like claims processing, customer service, sales and marketing efforts, and general corporate overhead. In 2023, Elevance reported total operating expenses of $151.6 billion, highlighting the scale of these expenditures.
Managing these operational costs efficiently is paramount for maintaining profitability in the competitive health insurance landscape. For instance, investments in technology to streamline claims processing and enhance customer service directly impact the bottom line. The company's focus on operational efficiency aims to control these outlays while delivering value to members.
Elevance Health significantly allocates resources to technology and digital advancements. In 2024, the company continued its substantial investments in IT infrastructure, the development of sophisticated digital platforms, and the integration of artificial intelligence and advanced data analytics capabilities. These strategic outlays are crucial for driving innovation, streamlining operational processes through automation, and ultimately elevating the experience for their members.
Provider Network Management Costs
Elevance Health incurs significant costs in managing its vast provider network. These expenses cover essential activities like negotiating contracts with hospitals and doctors, verifying their qualifications through credentialing processes, and maintaining positive relationships. This infrastructure is crucial for ensuring Elevance Health members have access to necessary medical services.
These provider network management costs are a substantial component of Elevance Health's operational expenses. For instance, in 2023, the company reported total operating expenses of $232.3 billion. While specific breakdowns for provider network management aren't always itemized separately in public reports, these activities directly contribute to the overall cost of delivering healthcare services.
- Contract Negotiations: Costs associated with legal teams and personnel dedicated to securing favorable terms with healthcare providers.
- Credentialing: Expenses related to verifying the licenses, certifications, and qualifications of physicians and facilities.
- Provider Relations: Investments in staff and systems to support and communicate with network providers, ensuring smooth operations and member satisfaction.
Salaries and Employee Benefits
Salaries and employee benefits constitute a significant portion of Elevance Health's cost structure due to its extensive workforce across various operational levels. This includes compensation for a broad spectrum of employees, ranging from frontline clinical professionals to administrative and executive management.
As a major player in the healthcare industry, Elevance Health's personnel expenses are substantial. For instance, in 2023, the company reported total operating expenses of $236.9 billion, a significant portion of which is attributable to employee-related costs. These costs are essential for maintaining the quality of care and operational efficiency across its diverse business segments.
- Salaries and Wages: Direct compensation for all employees, including clinical staff, administrative personnel, and leadership.
- Employee Benefits: Costs associated with health insurance, retirement plans, paid time off, and other benefits provided to employees.
- Training and Development: Investments in upskilling and professional development for the workforce to ensure competency and adaptation to industry changes.
- Payroll Taxes and Related Expenses: Employer contributions to social security, unemployment insurance, and other statutory payroll taxes.
Medical benefit expenses are the largest cost driver for Elevance Health, directly tied to member healthcare utilization and the cost of medical services. In 2024, these costs represented a significant portion of the company's revenue, underscoring the importance of managing care delivery expenses effectively.
Administrative and operating expenses, including claims processing and customer service, are also substantial. Elevance Health reported total operating expenses of $232.3 billion in 2023, highlighting the scale of these foundational business costs.
Investments in technology and digital platforms are a growing cost area, crucial for operational efficiency and member experience. Furthermore, managing its extensive provider network, involving contract negotiations and credentialing, incurs significant costs to ensure member access to care.
| Cost Category | 2023 Expense (Billions USD) | Key Components |
|---|---|---|
| Medical Benefit Expenses | (Not explicitly itemized, but largest component of total expenses) | Payments to providers for services |
| Operating Expenses | $232.3 | Claims processing, customer service, sales & marketing, G&A |
| Technology & Digital Investments | (Significant ongoing investment) | IT infrastructure, AI, data analytics |
| Provider Network Management | (Included within operating expenses) | Contract negotiation, credentialing, provider relations |
Revenue Streams
Elevance Health's core revenue is generated through health plan premiums. These premiums are collected from a diverse customer base, including individuals purchasing coverage directly, employers offering benefits to their employees, and government entities for programs like Medicare and Medicaid.
In 2023, Elevance Health reported total revenue of $171.8 billion, with a significant portion derived from these health insurance premiums across its various plan offerings. This demonstrates the sheer scale of their premium-based revenue model.
Elevance Health earns revenue through Administrative Services Only (ASO) fees. This involves managing the healthcare administration for self-funded employers who cover their employees' medical claims directly.
These ASO fees are charged for Elevance Health's expertise in network management, claims processing, and a suite of other essential administrative tasks, ensuring smooth operations for these employers.
In 2024, the market for ASO services continued to grow, with many large employers opting for these solutions to control costs and gain flexibility in their employee benefits programs.
Elevance Health's CarelonRx product and service revenue stems from its robust pharmacy benefit management (PBM) operations. This segment is a significant revenue driver, encompassing the sale of prescription medications and a suite of associated pharmacy services.
In 2024, CarelonRx demonstrated continued strength, contributing a substantial portion to Elevance Health's overall financial performance. This growth underscores the increasing demand for integrated pharmacy solutions and efficient drug cost management.
Carelon Services Revenue (Risk-Based Capabilities and Acquisitions)
Carelon Services, a key component of Elevance Health, draws revenue from a multifaceted approach centered on risk-based capabilities and strategic acquisitions. This segment’s income is largely derived from managing healthcare populations under various risk-sharing arrangements, where Carelon assumes a portion of the financial risk associated with patient care.
The company’s expansion into direct care delivery and the integration of acquired businesses significantly bolster its revenue streams. These acquisitions are not merely about scale but about deepening capabilities in areas like pharmacy benefit management and behavioral health, thereby creating more comprehensive service offerings.
- Risk-Based Care Management: Revenue generated from managing health outcomes and costs for defined patient populations, often through capitated payments or shared savings models.
- Acquired Capabilities: Income from newly integrated businesses, such as pharmacy benefit managers (PBMs) and specialty health services, expanding Carelon's market reach and service breadth.
- Integrated Health Services: Revenue from providing end-to-end healthcare solutions, encompassing everything from primary care to specialized treatment and administrative support.
- Pharmacy Services: Significant revenue contribution from Carelon's PBM operations, including drug dispensing, formulary management, and rebate negotiations.
Net Investment Income and Other Fees
Elevance Health diversifies its income beyond premiums through net investment income generated from its substantial financial asset portfolio. In 2023, the company reported significant investment income, contributing to its overall financial strength and providing a buffer against market volatility.
Further revenue streams are derived from a variety of specialized insurance offerings. These include dental, vision, and disability benefits, which cater to specific client needs and expand Elevance Health's market reach. These ancillary services represent a growing segment of their business.
- Net Investment Income: Earnings from the company's investments in securities and other financial instruments.
- Ancillary Services Fees: Revenue generated from specialized insurance products like dental, vision, and disability coverage.
- Diversification Benefit: These multiple revenue streams reduce reliance on core health insurance premiums, enhancing financial stability.
Elevance Health's revenue streams are robust and diversified, anchored by health plan premiums collected from individuals, employers, and government programs. In 2023, the company's total revenue reached $171.8 billion, highlighting the significant contribution of these premiums.
Beyond core insurance, Elevance Health generates substantial income from its CarelonRx pharmacy benefit management (PBM) operations, which include prescription sales and associated services. Furthermore, Administrative Services Only (ASO) fees from self-funded employers managing their own claims represent another key revenue source, with this market showing continued growth in 2024.
The company also benefits from net investment income on its financial assets and revenue from ancillary services like dental and vision coverage. Carelon Services contributes through risk-based care management and the integration of acquired businesses, expanding its integrated health solutions.
| Revenue Stream | Description | 2023 Impact (Illustrative) |
| Health Plan Premiums | Core income from insurance coverage. | Major contributor to $171.8B total revenue. |
| CarelonRx (PBM) | Pharmacy services and drug sales. | Significant growth driver in 2024. |
| ASO Fees | Administrative services for self-funded employers. | Growing market segment. |
| Net Investment Income | Earnings from financial assets. | Contributed to overall financial strength in 2023. |
| Ancillary Services | Dental, vision, disability benefits. | Expands market reach. |
Business Model Canvas Data Sources
The Elevance Health Business Model Canvas is built upon a foundation of comprehensive market research, internal operational data, and financial disclosures. These sources provide the necessary insights to accurately define customer segments, value propositions, and revenue streams.