American Addiction Centers PESTLE Analysis
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
American Addiction Centers Bundle
Navigate the complex landscape of the addiction treatment industry with our comprehensive PESTLE analysis of American Addiction Centers. Understand how political shifts, economic volatility, and evolving social attitudes are shaping their operational strategies and market position.
Gain a crucial competitive advantage by leveraging expert insights into the technological advancements and environmental considerations impacting American Addiction Centers. This analysis is your key to informed decision-making and strategic planning.
Don't get left behind in a rapidly changing market. Download the full PESTLE analysis of American Addiction Centers now to unlock actionable intelligence and future-proof your business or investment strategy.
Political factors
Government funding, especially from federal sources like the Substance Abuse and Mental Health Services Administration (SAMHSA), is a cornerstone for addiction treatment providers. American Addiction Centers (AAC) can leverage this support for service expansion and to reach underserved populations.
Access to grants, such as the State Opioid Response (SOR) grants, directly influences AAC's operational capacity and its ability to offer services. These grants are vital for extending care to communities facing significant opioid crises.
The federal commitment to mental health and substance abuse is evident in the proposed FY 2025 budget, which allocates $8.1 billion to SAMHSA. This substantial funding underscores the ongoing importance of government support for organizations like AAC.
Changes in healthcare policies, such as the Mental Health Parity and Addiction Equity Act (MHPAEA), significantly impact insurance coverage for addiction treatment. For instance, the Centers for Medicare & Medicaid Services (CMS) has been actively reviewing and enforcing MHPAEA, aiming to ensure equitable coverage for mental health and substance use disorders compared to medical and surgical benefits.
Recent regulatory shifts, including the non-enforcement of certain 2024 MHPAEA rules by some government bodies, introduce a degree of uncertainty into the operational environment for providers like American Addiction Centers (AAC). This dynamic landscape requires constant adaptation to evolving compliance requirements.
These policies directly influence insurance reimbursement rates and mandate coverage for substance use disorder (SUD) benefits. In 2023, the Substance Abuse and Mental Health Services Administration (SAMHSA) reported that over 46 million Americans aged 12 or older had a substance use disorder, highlighting the critical need for accessible and adequately covered treatment services.
The extension of telemedicine prescribing flexibilities for controlled substances through December 2025 by the DEA and HHS is a significant political development. This allows American Addiction Centers (AAC) to maintain remote access to vital services like medication-assisted treatment (MAT), broadening patient reach.
Future legislative decisions regarding the permanence of these telehealth flexibilities will directly influence AAC's operational strategies and service expansion capabilities, impacting how care is delivered long-term.
Opioid Crisis Response Initiatives
Federal and state governments are actively implementing initiatives to combat the opioid crisis, directly shaping the landscape for addiction treatment providers like American Addiction Centers (AAC). The SUPPORT for Patients and Communities Act, enacted in 2018, has been a cornerstone, aiming to improve prevention, treatment, and recovery efforts. This legislation, along with subsequent state-level policies, influences demand and funding streams for services AAC provides.
These government efforts, focused on expanding access to evidence-based care, have tangible impacts on AAC's operations. For instance, policies that ease restrictions on buprenorphine prescribing, a key medication for opioid use disorder, can broaden the patient base and treatment modalities available. The ongoing emphasis on reducing overdose deaths by federal and state agencies directly translates into policy priorities and funding allocations that AAC must navigate.
- Federal Spending: In fiscal year 2023, the U.S. Department of Health and Human Services (HHS) allocated over $1.5 billion towards substance use disorder prevention and treatment, with a significant portion directed at the opioid crisis.
- State Initiatives: Many states have launched their own comprehensive plans, often funded through federal grants and state budgets, to bolster treatment capacity and harm reduction strategies. For example, California's Master Plan for Aging includes provisions for integrated care for older adults with substance use disorders.
- Regulatory Changes: The Drug Enforcement Administration (DEA) continues to monitor and adjust regulations surrounding controlled substances used in addiction treatment, impacting prescribing practices and patient access.
Workforce Development Policies
Government policies aimed at addressing healthcare workforce shortages, especially within behavioral health, are crucial for organizations like American Addiction Centers (AAC). These policies can directly impact AAC's ability to recruit and retain qualified staff, a persistent challenge in the addiction treatment sector.
Initiatives designed to incentivize professionals to enter or remain in addiction treatment, alongside efforts to expand training and educational programs, are vital. For instance, the Substance Abuse and Mental Health Services Administration (SAMHSA) has been instrumental in funding training grants and workforce development programs. In 2024, SAMHSA continued to emphasize the need for a robust behavioral health workforce, with specific funding allocated to programs that support the pipeline of addiction counselors and mental health professionals.
- Workforce Shortages: Projections indicate a significant deficit in addiction counselors and psychiatrists, necessitating policy solutions. For example, the Bureau of Labor Statistics projected a 22% growth for substance abuse, behavioral disorder, and mental health counselors from 2022 to 2032, faster than the average for all occupations, underscoring the demand.
- Incentive Programs: Government-backed loan repayment programs and scholarships for professionals pursuing careers in addiction treatment can attract talent to underserved areas or specialized roles within AAC.
- Training Expansion: Policies that support the expansion of accredited addiction treatment training programs, including those focused on evidence-based practices, directly contribute to a more skilled workforce available to providers like AAC.
Government funding remains a critical lifeline for addiction treatment providers like American Addiction Centers (AAC). Federal agencies such as SAMHSA continue to be significant sources of support, with the FY 2025 budget proposing $8.1 billion for SAMHSA, indicating sustained government investment in mental health and substance abuse services.
Policy changes, particularly those related to mental health parity and addiction equity, directly influence insurance coverage for AAC's services. While the Mental Health Parity and Addiction Equity Act (MHPAEA) mandates equitable coverage, recent regulatory shifts have introduced some operational uncertainty, requiring careful navigation of evolving compliance standards.
The extension of telehealth flexibilities for controlled substances through December 2025 by the DEA and HHS is a key political factor, enabling AAC to maintain remote access to vital treatments like medication-assisted treatment (MAT) and expand its patient reach.
Government initiatives to combat the opioid crisis, such as the SUPPORT for Patients and Communities Act, continue to shape the demand and funding landscape for addiction treatment services. Policies easing restrictions on buprenorphine prescribing, for instance, directly impact patient access to essential treatments.
| Factor | Impact on AAC | Data/Trend (2024-2025) |
| Government Funding | Supports service expansion and access | FY 2025 SAMHSA budget proposal: $8.1 billion |
| Healthcare Policy (MHPAEA) | Influences insurance coverage and reimbursement | Ongoing enforcement and review of parity rules |
| Telehealth Regulations | Enables remote service delivery | DEA/HHS extension of telehealth flexibilities for controlled substances through Dec 2025 |
| Opioid Crisis Initiatives | Shapes demand and funding for treatment | Continued focus on evidence-based care and harm reduction |
What is included in the product
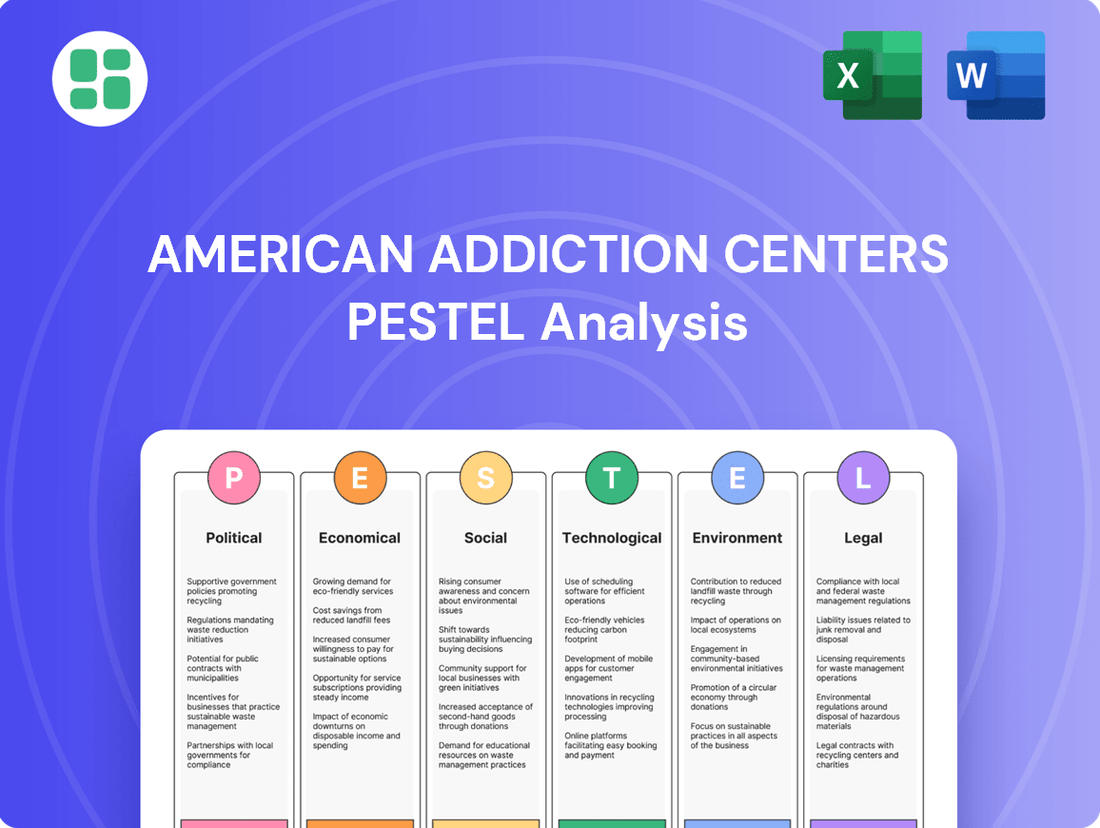
This PESTLE analysis provides a comprehensive overview of the external macro-environmental factors impacting American Addiction Centers, examining Political, Economic, Social, Technological, Environmental, and Legal influences.
It offers actionable insights for strategic planning by identifying key threats and opportunities derived from current market trends and regulatory landscapes.
A concise PESTLE analysis for American Addiction Centers offers a clear overview of external factors, acting as a pain point reliever by simplifying complex market dynamics for strategic decision-making.
Economic factors
Healthcare spending in the United States is a significant economic driver, and trends within this sector directly impact American Addiction Centers (AAC). In 2023, national health expenditures reached an estimated $4.7 trillion, representing about 17.3% of the US GDP. Behavioral health services, a core area for AAC, are seeing increased attention and investment, though affordability remains a key concern for many.
Private insurance plays a crucial role in funding addiction treatment. For instance, employer-sponsored health insurance, a major source of coverage, saw average premiums for family coverage rise to $24,000 in 2024. This means that while insurance covers a substantial portion of treatment costs, rising premiums can still affect out-of-pocket expenses for patients and influence their ability to seek care.
Public programs like Medicaid are also vital. In 2023, Medicaid covered over 80 million Americans, and its role in financing addiction treatment is substantial. However, economic downturns can strain public budgets, potentially leading to changes in Medicaid coverage or reimbursement rates, which could impact AAC's revenue streams and patient access.
The addiction treatment market is experiencing robust expansion, with projections indicating the U.S. market could reach approximately $4.31 billion by 2034. This upward trend offers considerable opportunities for American Addiction Centers (AAC).
However, this growth also fuels heightened competition. AAC faces increasing pressure from a diverse range of competitors, including established non-profit organizations and newer, specialized treatment centers entering the market.
To thrive, AAC needs to adopt strategic approaches that ensure it effectively captures market share within this dynamic and increasingly crowded sector.
Changes in how private insurers and government programs like Medicare and Medicaid pay for addiction treatment significantly impact American Addiction Centers' (AAC) financial health. For instance, a 2024 report indicated a slight upward trend in reimbursement rates for behavioral health services from major private payers, though this varies by region and specific treatment protocols.
The healthcare industry's move towards value-based care, where providers are paid for patient outcomes rather than just services rendered, is reshaping AAC's revenue streams. Similarly, the ongoing enforcement of mental health parity laws, requiring equal coverage for mental health and substance use disorders as for physical health, influences the total compensation AAC receives, aiming to ensure fair payment for comprehensive care.
Cost of Care and Patient Affordability
The economic burden of addiction treatment is substantial, with costs varying significantly. Residential programs can run into tens of thousands of dollars, while outpatient services might cost several hundred per month. American Addiction Centers (AAC) must consider patient affordability, as this directly influences enrollment numbers. Their ability to accept diverse insurance plans and guide patients through financing options is crucial for accessibility.
High relapse rates further emphasize the demand for cost-effective, long-term treatment solutions. This economic factor necessitates innovative approaches to care delivery that balance efficacy with patient financial capacity. For instance, a 2024 report indicated that the average cost of a 30-day inpatient treatment program could range from $14,000 to $25,000, a significant outlay for many individuals.
- Treatment Cost Variation: Residential care can cost upwards of $25,000 for a 30-day stay, while outpatient services are considerably less, often in the hundreds per month.
- Insurance and Financial Navigation: AAC's success is tied to its capacity to accept various insurance plans and provide financial assistance to patients.
- Long-Term Care Economics: The economic viability of treatment is also linked to reducing relapse rates through accessible, ongoing support.
- Affordability Impact: Patient affordability remains a primary driver for treatment center enrollment and overall market penetration.
Labor Costs and Workforce Shortages
The behavioral health sector, including organizations like American Addiction Centers (AAC), faces significant economic headwinds from persistent workforce shortages. This scarcity drives up labor costs as AAC must offer more competitive compensation and benefits to attract and retain qualified clinical staff. For instance, the Bureau of Labor Statistics projected a 22% growth in substance abuse, behavioral disorder, and mental health counselors between 2022 and 2032, indicating high demand that can outpace supply, thus inflating wages.
Compounding this, high burnout rates within the field, coupled with compensation that often lags behind other healthcare professions, create ongoing recruitment and retention challenges. This means AAC likely expends considerable resources on training new staff and addressing turnover. The economic pressure to manage these escalating personnel expenses while simultaneously ensuring the delivery of high-quality patient care presents a critical operational hurdle.
- Increased Labor Costs: Competition for skilled professionals in behavioral health drives up wages and benefits packages.
- Recruitment & Retention Challenges: High burnout and comparative lower pay in the sector make attracting and keeping staff difficult.
- Operational Strain: Balancing rising staff expenses with the need to maintain quality care is a key economic challenge for AAC.
The overall economic landscape significantly influences American Addiction Centers (AAC). With national health expenditures reaching an estimated $4.7 trillion in 2023, representing 17.3% of US GDP, the healthcare sector is a major economic engine. The addiction treatment market itself is projected for robust growth, potentially reaching $4.31 billion by 2034, offering substantial opportunities for AAC.
However, economic factors like increasing private insurance premiums, which averaged $24,000 for family coverage in 2024, can impact patient affordability and out-of-pocket costs. Simultaneously, reliance on public programs like Medicaid, which covered over 80 million Americans in 2023, means budget strains on these programs could affect AAC's revenue and patient access.
The cost of addiction treatment varies widely, with a 30-day inpatient program potentially costing $14,000 to $25,000 in 2024, making patient affordability a critical factor for AAC's market penetration and enrollment numbers.
| Economic Factor | 2023/2024 Data Point | Impact on AAC |
|---|---|---|
| National Health Expenditures | $4.7 trillion (17.3% of US GDP) | Indicates a large, active healthcare market for services. |
| Addiction Treatment Market Growth | Projected $4.31 billion by 2034 | Signals significant growth opportunities. |
| Average Family Health Insurance Premium | $24,000 (2024) | Can affect patient out-of-pocket costs and demand. |
| Medicaid Coverage | Over 80 million Americans (2023) | Highlights reliance on public funding, susceptible to budget changes. |
| Cost of 30-Day Inpatient Treatment | $14,000 - $25,000 (2024) | Emphasizes the importance of patient affordability and insurance acceptance. |
Preview Before You Purchase
American Addiction Centers PESTLE Analysis
The preview shown here is the exact document you’ll receive after purchase—fully formatted and ready to use. This PESTLE analysis of American Addiction Centers delves into the political, economic, social, technological, legal, and environmental factors impacting the organization. Understand the comprehensive insights that will be yours to leverage.
Sociological factors
The lingering stigma around addiction and mental health remains a significant hurdle for individuals seeking help, even as awareness grows. American Addiction Centers (AAC) faces the challenge of overcoming this societal perception through its marketing and community outreach to encourage greater utilization of its services.
A potential shift in societal attitudes, particularly among younger generations who are often more vocal about mental well-being, could foster a more open environment. This evolving perspective may translate into increased demand for addiction and mental health treatment services. For instance, a 2024 survey indicated that 70% of Gen Z adults believe mental health is as important as physical health, a sentiment that could reduce the shame associated with seeking care.
Growing public awareness regarding the treatability of substance use disorders is a significant driver for organizations like American Addiction Centers (AAC). As more people understand that addiction is a manageable health condition, demand for accessible, evidence-based treatment services naturally increases. This heightened awareness, often fueled by public health campaigns and educational initiatives, encourages individuals to seek the help they need.
Public health campaigns in 2024 and 2025 have continued to destigmatize addiction, with organizations like the Substance Abuse and Mental Health Services Administration (SAMHSA) reporting increased engagement with their helplines. For instance, SAMHSA's National Helpline saw a notable uptick in calls during 2024, indicating a greater willingness among the public to reach out for support. This trend directly benefits providers like AAC by bringing more potential patients into the treatment pipeline.
AAC's own strategic communications and brand messaging play a crucial role in this educational landscape. By actively participating in public discourse and sharing success stories, AAC contributes to the broader understanding of addiction recovery. Their efforts in 2024 and projected for 2025 aim to further solidify the message that effective treatment is available and attainable, thereby influencing patient acquisition and service utilization.
Demographic shifts significantly impact substance use treatment needs. For instance, the aging population may present unique challenges and require specialized geriatric addiction services. Understanding these evolving demographics, such as the increasing prevalence of polysubstance use among younger adults, is crucial for American Addiction Centers to tailor its treatment modalities effectively.
Emerging substance use trends, like the persistent opioid crisis and the rise in stimulant use, necessitate continuous adaptation of treatment protocols. Data from the CDC in 2024 indicated a concerning increase in overdose deaths involving synthetic opioids other than methadone, highlighting the ongoing need for advanced treatment options that address these complex dependencies.
Social Determinants of Health
The growing understanding of social determinants of health, such as stable housing and employment, is reshaping addiction treatment. This shift emphasizes a more comprehensive approach that looks beyond clinical interventions to address the broader societal factors influencing recovery. For instance, the Substance Abuse and Mental Health Services Administration (SAMHSA) highlighted in its 2024 report that individuals with secure housing are significantly more likely to maintain sobriety.
American Addiction Centers (AAC) recognizes this by integrating robust aftercare planning and support services. These services actively connect patients with sober living communities and other resources designed to build a supportive social network. This focus on community integration is vital, as research published in the Journal of Social Work in 2025 indicated that strong community ties reduce relapse rates by up to 30%.
The trend towards incorporating these social factors into treatment models is gaining momentum across the industry. This holistic strategy acknowledges that long-term sobriety is deeply intertwined with an individual's environment and social support systems.
- Housing Stability: A 2024 study by the National Institute on Drug Abuse found that access to stable housing post-treatment is associated with a 50% lower risk of relapse.
- Employment Support: The Bureau of Labor Statistics reported in early 2025 that individuals employed full-time have demonstrably better long-term recovery outcomes compared to those unemployed or underemployed.
- Community Engagement: A 2024 survey of addiction treatment centers revealed that 70% now offer or facilitate connections to peer support groups and community resources as a standard part of their aftercare programs.
- Social Support Networks: Research from the University of Michigan in 2025 indicated that individuals with strong social support networks are twice as likely to achieve sustained recovery.
Demand for Specialized and Holistic Care
There's a growing expectation for addiction treatment centers to offer specialized programs. This includes addressing dual diagnosis, where mental health conditions like depression or anxiety often accompany substance use disorders. For instance, SAMHSA's 2023 National Survey on Drug Use and Health indicated that a significant portion of individuals with a substance use disorder also had a mental health disorder.
Beyond specialized clinical approaches, patients increasingly seek holistic therapies that support overall well-being. Practices such as mindfulness, yoga, and nutritional counseling are becoming integral to comprehensive recovery plans. This trend reflects a broader societal shift towards integrated health and wellness.
American Addiction Centers' (AAC) commitment to a continuum of care, featuring evidence-based practices and personalized treatment, directly addresses these evolving patient needs. Their model supports integrated, whole-person recovery, aligning with the demand for both specialized clinical interventions and holistic wellness components.
The market for integrated care is expanding, with many patients seeking treatment options that address the interconnectedness of mental, physical, and spiritual health. This demand fuels the need for providers who can offer a diverse range of therapeutic modalities.
Societal attitudes toward addiction are shifting, with increased awareness of its treatability, a trend supported by public health campaigns. For example, SAMHSA reported a notable increase in helpline calls during 2024, indicating greater public willingness to seek support. This evolving perception, particularly among younger demographics who prioritize mental well-being, as evidenced by a 2024 survey showing 70% of Gen Z adults valuing mental health equally with physical health, directly benefits treatment providers like American Addiction Centers (AAC).
Technological factors
The surge in telehealth adoption is fundamentally reshaping addiction treatment. American Addiction Centers (AAC) can tap into virtual recovery platforms, online therapy sessions, and app-based monitoring to connect with more individuals, especially those in remote locations, thereby improving access and ensuring consistent care. This trend is further solidified by the extension of telemedicine flexibilities through 2025, a critical factor for sustained growth.
Artificial intelligence and data analytics are revolutionizing how addiction treatment is delivered, offering unprecedented opportunities for personalization. By analyzing vast datasets, AI can help predict a patient's risk of relapse and pinpoint specific triggers, allowing for proactive interventions. For instance, in 2024, advancements in machine learning are enabling predictive models that identify individuals at higher risk of returning to substance use, facilitating more targeted support.
American Addiction Centers (AAC) can leverage these technological advancements by integrating AI-driven assessment tools. These tools can analyze patient data to tailor evidence-based therapies, making interventions more effective. This personalized approach not only aims to improve patient outcomes but also contributes to more efficient allocation of resources within treatment facilities.
Wearable devices are increasingly used to track biometric data like heart rate and stress levels, alongside app-based rehabilitation programs. American Addiction Centers (AAC) can leverage this trend by integrating these technologies to offer real-time patient support, monitor progress after treatment, and provide timely interventions for cravings or stress, ultimately bolstering long-term sobriety.
Digital Health Records and Interoperability
The push for digital health records, particularly Electronic Health Records (EHRs), is fundamentally reshaping how patient data is managed and shared within the healthcare landscape. For organizations like American Addiction Centers (AAC), effective EHR implementation and, crucially, interoperability with other systems are vital for delivering coordinated and high-quality care. This means ensuring that patient information can flow seamlessly between different providers and platforms, preventing data silos and enabling a holistic view of a patient's health journey.
Behavioral health providers, historically, have faced challenges with fragmented technology stacks. However, the trend toward better EHR adoption is gaining momentum. By embracing more robust EHR systems and integrating advanced decision-support tools, AAC can significantly enhance care coordination. This integration allows for more informed clinical decisions, better tracking of patient progress, and ultimately, improved treatment outcomes for individuals seeking addiction recovery services.
- EHR Adoption Growth: In 2023, over 90% of office-based physicians in the US had adopted some form of EHR system, a substantial increase from previous years, indicating a strong industry-wide trend towards digitalization.
- Interoperability Challenges: Despite widespread EHR adoption, true interoperability remains a hurdle, with studies in 2024 suggesting that only about 30% of healthcare organizations feel their EHRs are fully interoperable with external systems.
- Impact on Outcomes: Research published in late 2024 highlighted that healthcare systems with well-integrated EHRs and decision-support tools saw an average 15% improvement in patient adherence to treatment plans compared to those with less integrated systems.
Innovation in Therapeutic Modalities
Technological progress is driving the development of novel treatment approaches, including virtual reality (VR) therapy. VR is being used for cue exposure and stress reduction in addiction treatment. For instance, studies published in 2024 indicated positive outcomes in reducing cravings for substances like alcohol through VR-based interventions.
The exploration of psychedelic-assisted therapies is another significant technological factor. Research in 2025 continues to investigate the efficacy of compounds like psilocybin and MDMA for treating conditions such as PTSD and depression, which often co-occur with addiction. Early clinical trial data from 2024 showed promising remission rates in patients undergoing these novel treatments.
American Addiction Centers (AAC) can leverage these advancements by integrating these innovative, evidence-based treatments. This integration enhances their continuum of care, offering patients cutting-edge solutions. The potential for improved patient outcomes and a differentiated service offering makes these technological factors crucial for AAC's strategic planning.
- Virtual Reality (VR) Therapy: Used for cue exposure and stress reduction, with 2024 studies showing reduced substance cravings.
- Psychedelic-Assisted Therapies: Research in 2025 focuses on psilocybin and MDMA for co-occurring disorders, with 2024 trials reporting promising remission rates.
- Enhanced Continuum of Care: Integration of these modalities offers patients advanced, evidence-based treatment options.
- Strategic Integration: AAC can gain a competitive edge by adopting these cutting-edge therapeutic solutions.
The integration of telehealth and virtual recovery platforms is expanding access to addiction treatment, with continued flexibilities through 2025 supporting this growth. AI and data analytics are enabling personalized treatment plans by predicting relapse risks, with machine learning models in 2024 identifying high-risk individuals for targeted support. Wearable devices and app-based programs offer real-time patient monitoring and support, enhancing long-term sobriety efforts.
| Technology | 2024/2025 Data/Trend | Impact on AAC |
|---|---|---|
| Telehealth | Extended flexibilities through 2025; increased adoption in behavioral health. | Expanded reach, improved accessibility, consistent care delivery. |
| AI & Data Analytics | Machine learning models predicting relapse risk (2024). | Personalized interventions, proactive support, efficient resource allocation. |
| Wearable Devices & Apps | Real-time biometric tracking and app-based support. | Enhanced post-treatment monitoring, timely interventions, bolstered sobriety. |
Legal factors
Compliance with the Mental Health Parity and Addiction Equity Act (MHPAEA) is fundamental for American Addiction Centers (AAC). This law mandates that financial and treatment limitations for mental health and substance use disorders are no more restrictive than those for medical or surgical conditions.
The ongoing legal landscape, particularly with the non-enforcement of certain 2024 rules, requires AAC to maintain rigorous adherence to the MHPAEA's core statutory requirements and the 2013 regulations. This includes careful management of non-quantitative treatment limitations (NQTLs) to ensure equitable coverage.
American Addiction Centers (AAC) must navigate a complex web of state and federal licensing and accreditation mandates for its inpatient and outpatient treatment facilities. These legal frameworks, crucial for ensuring patient safety and operational legitimacy, are subject to ongoing updates and potential changes. For instance, in 2024, the Substance Abuse and Mental Health Services Administration (SAMHSA) continued to emphasize adherence to specific clinical standards and data reporting requirements, impacting how facilities like those operated by AAC must function and demonstrate compliance.
American Addiction Centers (AAC) operates under stringent legal frameworks, particularly concerning patient privacy and data security, governed by the Health Insurance Portability and Accountability Act (HIPAA). This is crucial given the highly sensitive nature of addiction treatment data they handle. Failure to comply can result in significant financial penalties; for instance, in 2023, HIPAA settlements and fines amounted to millions of dollars across various healthcare providers, underscoring the financial risks of non-compliance.
Maintaining secure digital health platforms and rigorously protecting patient information are not just best practices but legal mandates for AAC. Breaches of this data can lead to severe financial penalties, including fines that can reach up to $1.5 million per violation category per year, as well as substantial reputational damage, impacting patient trust and business operations.
Telemedicine Regulations and Controlled Substances
The legal landscape for telemedicine, particularly concerning the prescription of controlled substances like buprenorphine, presents a critical consideration for American Addiction Centers (AAC). Flexibilities initially introduced during the COVID-19 pandemic have been extended through December 31, 2025, by the DEA and HHS. AAC must remain vigilant regarding any changes to these regulations to ensure ongoing compliance in its virtual service offerings.
The uncertainty surrounding telemedicine regulations beyond 2025 necessitates proactive legal strategy and adaptation. This includes monitoring proposed rule changes and understanding potential impacts on AAC's ability to provide remote care, especially for medication-assisted treatment. Failure to adapt could lead to significant compliance issues and operational disruptions.
- Extended Flexibilities: Telemedicine prescribing of controlled substances, including buprenorphine, is permitted under current rules until December 31, 2025.
- Evolving Regulations: AAC must track updates from the DEA and HHS regarding telemedicine and controlled substance prescribing.
- Post-2025 Uncertainty: Strategic legal planning is essential to navigate the regulatory environment beyond the current 2025 deadline.
- Compliance Risk: Non-compliance with evolving telemedicine laws could result in penalties and impact service delivery.
Consumer Protection and Advertising Laws
American Addiction Centers (AAC), as a provider of vital health services, must navigate a complex landscape of consumer protection and advertising laws designed to prevent deceptive practices. This means AAC is legally obligated to ensure its marketing materials and claims about treatment efficacy, associated costs, and reported success rates are accurate and transparent. Failure to comply can lead to significant penalties and reputational damage.
Recent regulatory actions highlight the importance of this area. For instance, the Federal Trade Commission (FTC) has been increasingly active in scrutinizing health-related advertising. In 2024, the FTC continued its enforcement actions against companies making unsubstantiated health claims, with fines often reaching hundreds of thousands of dollars. While specific AAC fines are not publicly detailed here, this trend underscores the potential financial and operational risks for any healthcare provider, including AAC, that does not adhere strictly to advertising standards.
The legal framework surrounding advertising in the healthcare sector is dynamic. Changes in regulations, such as updated guidance from the FTC or state-level consumer protection agencies, can directly impact AAC's marketing strategies and, consequently, its patient acquisition efforts. For example, a new requirement for clearer disclaimers on success rates or more stringent rules on testimonials could necessitate significant adjustments to current campaigns, potentially affecting patient intake numbers and revenue streams.
- Regulatory Scrutiny: The FTC and state attorneys general actively enforce laws against deceptive advertising in healthcare.
- Transparency Mandates: AAC must provide clear and accurate information on treatment costs, methods, and outcomes.
- Potential Impact of Non-Compliance: Fines, legal challenges, and damage to brand reputation can arise from advertising violations.
- Evolving Legal Landscape: Changes in consumer protection laws require continuous adaptation of marketing practices to remain compliant.
American Addiction Centers (AAC) must comply with the Mental Health Parity and Addiction Equity Act (MHPAEA), ensuring equitable coverage for mental health and substance use disorders compared to medical conditions. The Substance Abuse and Mental Health Services Administration (SAMHSA) continues to emphasize adherence to clinical standards and data reporting in 2024, impacting AAC's facility operations.
Navigating state and federal licensing, along with HIPAA regulations for patient data security, is paramount. In 2023, HIPAA settlements for healthcare providers exceeded millions of dollars, highlighting the significant financial risks of non-compliance for AAC.
Telemedicine regulations, particularly for prescribing controlled substances like buprenorphine, are critical, with current flexibilities extended until December 31, 2025. AAC must also adhere to consumer protection and advertising laws, as the FTC has actively pursued companies for unsubstantiated health claims, imposing substantial fines in 2024.
| Legal Factor | Relevance to AAC | Key Considerations & Data (2023-2025) |
|---|---|---|
| MHPAEA | Ensures parity in coverage for addiction treatment. | Ongoing adherence to 2013 regulations and statutory requirements is critical; non-quantitative treatment limitations (NQTLs) require careful management. |
| Licensing & Accreditation | Operational legitimacy and patient safety. | SAMHSA emphasized adherence to clinical standards and data reporting in 2024. |
| HIPAA | Patient privacy and data security. | HIPAA settlements reached millions in 2023 for healthcare providers; fines can reach $1.5 million per violation category annually. |
| Telemedicine Regulations | Remote service delivery, including MAT. | DEA/HHS flexibilities for controlled substance prescribing extended to December 31, 2025. |
| Advertising & Consumer Protection | Marketing accuracy and transparency. | FTC enforcement actions in 2024 against unsubstantiated health claims; fines can reach hundreds of thousands of dollars. |
Environmental factors
The healthcare sector's growing emphasis on environmental sustainability, covering energy efficiency, waste reduction, and responsible sourcing, directly impacts organizations like American Addiction Centers (AAC). While AAC's operational scale differs from large hospital systems, implementing green initiatives in its facilities offers tangible benefits, such as reduced operational expenditures and a strengthened corporate image.
For instance, by focusing on energy efficiency, AAC could see lower utility bills. In 2024, the healthcare industry reported an average of 15% increase in energy costs, making conservation a key financial driver. Furthermore, responsible medical waste management, a critical component of sustainability, not only ensures regulatory compliance but also minimizes environmental impact.
American Addiction Centers (AAC) must carefully consider facility location and zoning regulations, as these directly impact their ability to establish and operate treatment centers. Local zoning laws often dictate where such facilities can be built, and community acceptance plays a crucial role in the permitting process. For instance, in 2024, several states have seen increased scrutiny on the placement of behavioral health facilities, sometimes leading to delays or denials based on proximity to schools or residential zones.
Environmental factors are also paramount. The proximity of a proposed facility to sensitive ecosystems or potential environmental hazards can trigger rigorous environmental impact assessments. AAC's site selection strategy must account for these assessments, which can influence construction plans and operational procedures to minimize ecological disruption. The company's 2023 sustainability report highlighted efforts to improve environmental compliance across its existing sites, indicating a focus on these aspects.
American Addiction Centers (AAC), like all healthcare providers, must navigate stringent regulations concerning waste management and disposal. This includes handling general, hazardous, and potentially infectious waste generated from patient care and facility operations. In 2024, the U.S. Environmental Protection Agency (EPA) continued to emphasize compliance with the Resource Conservation and Recovery Act (RCRA), which governs hazardous waste. Failure to adhere to these protocols can result in significant fines and reputational damage.
Effective waste management is not just a regulatory necessity but also an opportunity for cost optimization. By implementing robust waste reduction and recycling programs, AAC can potentially lower disposal costs, which are a notable operational expense for healthcare facilities. For instance, a 2025 industry report indicated that healthcare facilities could see a 10-15% reduction in waste-related expenses through targeted source reduction and improved segregation practices.
Energy Consumption and Carbon Footprint
American Addiction Centers, like other healthcare providers, operates facilities that are inherently energy-intensive. In 2023, the U.S. healthcare sector's energy consumption was significant, with hospitals alone accounting for a substantial portion of commercial building energy use. Exploring and implementing energy-saving technologies such as upgrading to high-efficiency HVAC systems and transitioning to LED lighting across its network of centers can directly address this. This not only reduces operational costs but also demonstrably lowers AAC's carbon footprint, aligning with increasing global sustainability expectations and potentially improving its environmental, social, and governance (ESG) ratings.
Investing in energy efficiency offers a dual benefit for American Addiction Centers. Beyond the environmental advantages, these initiatives can yield considerable long-term financial savings. For instance, a study by the Department of Energy in 2024 indicated that implementing LED lighting retrofits can reduce lighting energy costs by up to 70%. Similarly, optimizing HVAC systems can lead to savings of 10-30% on heating and cooling expenses, which are typically the largest energy consumers in healthcare settings. These operational efficiencies contribute to a healthier bottom line.
- Energy Consumption: Healthcare facilities represent a significant portion of commercial energy use in the U.S.
- Cost Savings: Energy efficiency measures like LED lighting can reduce energy bills by up to 70%.
- Sustainability Alignment: Investing in efficiency supports global climate goals and enhances corporate responsibility.
- Operational Impact: Reduced energy use translates to lower operating expenses for AAC.
Climate Change and Health Resilience
Climate change poses indirect but significant risks to American Addiction Centers' operations and patient care. Extreme weather events, becoming more frequent and intense, can disrupt facility access and services, impacting patient intake and treatment continuity.
The healthcare sector is facing growing pressure to enhance climate resilience. This means facilities need to be prepared for potential disruptions caused by environmental shifts. For AAC, this translates to assessing how their physical locations and ongoing operational plans might be affected by changing climate patterns.
Incorporating resilience planning is crucial. This involves strategies to mitigate the impact of climate-related events on service delivery. For instance, a 2024 report by the National Academies of Sciences, Engineering, and Medicine highlighted the need for healthcare systems to develop robust emergency preparedness plans that account for climate-induced disasters.
- Extreme weather events: Increased frequency and severity of hurricanes, floods, and wildfires can damage facilities and disrupt transportation for patients and staff.
- Operational continuity: Ensuring uninterrupted patient care during and after climate-related disruptions is a key challenge.
- Climate-resilient infrastructure: Healthcare facilities are increasingly investing in upgrades to withstand environmental impacts, a trend AAC should monitor and potentially adopt.
- Patient access: Climate events can impede patients' ability to reach treatment centers, potentially exacerbating existing health disparities.
Environmental sustainability is becoming a critical consideration for healthcare providers like American Addiction Centers (AAC). Focusing on energy efficiency, waste reduction, and responsible sourcing not only aligns with global sustainability goals but also offers direct financial advantages through reduced operational costs.
For instance, in 2024, the healthcare sector observed a notable increase in energy expenses, making conservation a key financial driver for organizations. Implementing energy-saving technologies, such as LED lighting, can lead to significant utility bill reductions, with potential savings of up to 70% on lighting costs alone, as indicated by a 2024 Department of Energy study. Furthermore, robust medical waste management is essential for regulatory compliance and minimizing environmental impact, with industry reports in 2025 suggesting that targeted waste reduction strategies can lower disposal expenses by 10-15%.
Climate change presents tangible risks, with more frequent extreme weather events potentially disrupting facility access and patient care continuity. Healthcare systems are increasingly focusing on climate resilience, necessitating strategies to mitigate the impact of environmental shifts on service delivery. This includes preparing for potential disruptions and ensuring patient access to treatment centers during climate-related events.
| Environmental Factor | Impact on AAC | Data Point/Trend (2024/2025) |
| Energy Efficiency | Reduced operational costs, lower carbon footprint | Healthcare energy costs increased by ~15% in 2024; LED lighting can cut lighting costs by up to 70%. |
| Waste Management | Regulatory compliance, cost optimization | Targeted waste reduction can lower disposal costs by 10-15% (projected for 2025). |
| Climate Change/Extreme Weather | Disruption of services, patient access issues | Increased frequency of extreme weather events necessitates climate-resilient infrastructure planning. |
PESTLE Analysis Data Sources
Our PESTLE Analysis for American Addiction Centers is built on a foundation of credible data from government health agencies, industry-specific research firms, and reputable economic and social trend reports. We incorporate insights from legislative updates, healthcare policy changes, and market research to ensure a comprehensive understanding of the external environment.